Physicians frequently encounter acute and primary care patients complaining of skin changes or lesions. Swift initiation of proper treatment and pharmacotherapy for patients with rashes is essential to prevent complications, morbidity, and excessive use of hospital resources [1,3]. Sweet syndrome, or Acute Febrile Neutrophilic Dermatosis, is a rare and highly symptomatic inflammatory skin condition. Recognizing Sweet syndrome early is crucial, as it necessitates specific treatment approaches and can often signal an underlying pro-inflammatory disease, malignancy, or a reaction to new medication. This case report explores the presentation and management of a 50-year-old male exhibiting a classic presentation of sweet syndrome.
Introduction

Physicians frequently encounter patients with skin changes or lesions in acute care. Recognizing these concerning rashes and skin alterations is crucial for physicians, as mis-triage and misdiagnosis can lead to various consequences, from unfavorable patient outcomes to excessive utilization of hospital resources3,4. For patients exhibiting skin changes, prompt initiation of appropriate therapy is essential, particularly for those at risk of decompensation, experiencing significant symptoms, or potentially harboring a serious underlying medical condition with skin manifestations. Acute febrile neutrophilic dermatosis, also known as sweet syndrome, is a rare inflammatory skin condition linked to pro-inflammatory diseases, hematologic or oncologic malignancies, and the introduction of new medications1,2.
Case Presentation: A 50-year-old male with Skin Lesions1

Figure 1: Raised, erythematous, painful, Nikolsky-negative, hemorrhagic, bullous skin lesions of the hands that spared the palms
- Patient Background
- Age: 50 years
- Medical History: Chronic obstructive pulmonary disease, hepatitis C, end-stage renal disease on dialysis
- Timeline of Symptoms
- Onset: Skin lesions appeared one week before the ED presentation
- Initial Treatment: Previously treated with intravenous antibiotics at another hospital
- Progression: Lesions enlarged and spread diffusely, leading to the ED visit
- Clinical Examination
- Vital Signs: Normal
- General Condition: The patient appeared uncomfortable
- Skin Findings
- Polymorphic, raised, hemorrhagic, bullous lesions
- Heaped margins
- Intraoral mucosa involvement
- Nikolsky sign negative
- Lesions spared palms and soles (Figure 1)
- Diagnostic Testing
- Tests Conducted: Monkeypox, herpes simplex virus, varicella-zoster virus Blood cultures, gonorrhea/chlamydia, HIV, RPR, hepatitis panel
- Results
- All tests were negative except for positive hepatitis C RNA
- White blood cell count: 5,000/µL
- C-reactive protein: 159 mg/L
- Management and Admission
- Concerns: Systemic and highly symptomatic skin changes
Potential concurrent infection or underlying occult disease - Action: Admitted for further evaluation
Empirically started on broad-spectrum antibiotics and high-dose intravenous steroids
- Concerns: Systemic and highly symptomatic skin changes
- Diagnostic Workup and Treatment
Inpatient Team’s Investigations
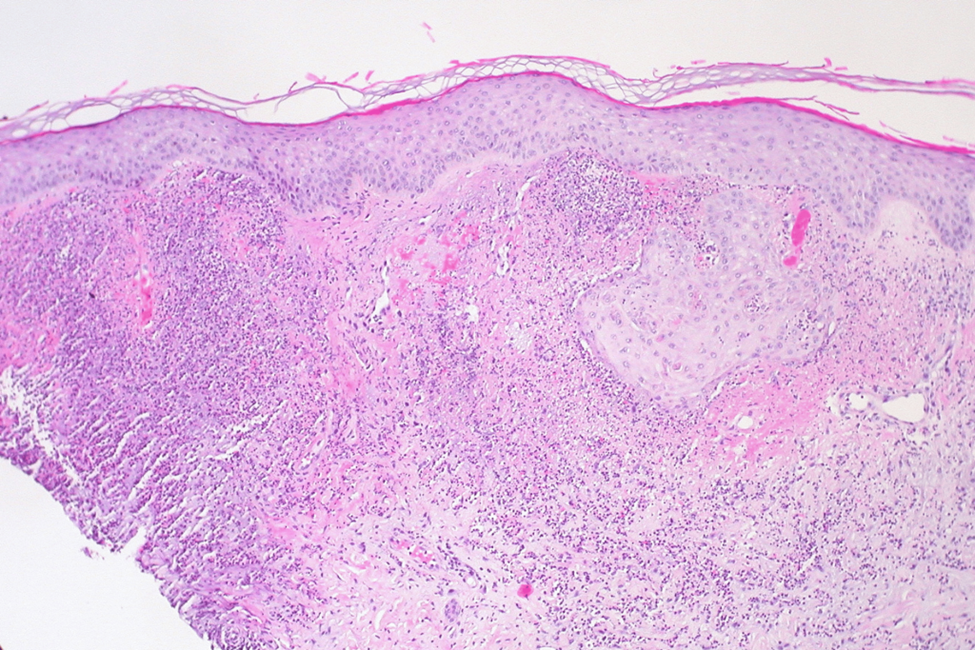
Figure 2: Histopathology slide of a patient’s skin biopsy showing neutrophils in the upper dermis with a fibrinoid change of capillary-sized vessels consistent with a diagnosis of Sweet syndrome- Objective: Identify underlying infectious, autoimmune, and oncologic diseases
- Tests Conducted
- Cryptococcal antigens
- Blastomyces antibodies
- Histoplasma antibodies
- Screening chest, abdomen, and pelvis computed tomography
- Microorganism testing of lesion biopsy
- Test Results
- Outcome: All tests were negative
- Skin Biopsy Findings: Collections of neutrophils in the upper dermis
- Fibrinoid change of capillary-sized vessels
- Negative microorganism testing
- Consistent with acute febrile neutrophilic dermatosis (Sweet syndrome) (Figure 2)
- Treatment Initiation
- Antibiotics Discontinued
- Prednisone Dose: 1 mg/kg
- Reasoning: Diagnosis confirmation and symptom management
- Patient Progress
- Hospital Course: Four days
- Symptom Improvement: Significant
- Discharge Plan: Oral prednisone taper
- Follow-Up: Specialty follow-up is arranged
Discussion
Physicians frequently encounter patients in the acute care setting with skin issues of unknown origin. Healthcare providers must discern when immediate treatment and further inpatient management are necessary for a skin condition or if it may indicate an underlying occult disease process. Misdiagnosis can lead to inappropriate treatment, delayed treatment causing increased morbidity, or failure to identify a serious, mysterious disease requiring intervention. One such condition is sweet syndrome, often linked to underlying infection or malignancy [1]. Robert Sweet first described it in 1964, identifying skin eruptions resembling erythema multiforme associated with fever in eight cases.
The diagnosis of sweet syndrome involves major criteria (abrupt onset of painful erythematous plaques and nodules, and histopathologic evidence of dense neutrophilic infiltrate without leukocytoclastic vasculitis) and two of four minor criteria (fever, known malignancy or infection, elevated inflammatory markers, and excellent response to systemic steroids) [1,2,4]. High-dose corticosteroid therapy is the primary treatment, with topical or intralesional injections recommended for mild cases and systemic treatment for extensive/systemic disease. Colchicine, dapsone, and potassium iodide are less commonly used but still employed [1,4]. Our patient had the rare bullous form of sweet syndrome, often associated with an underlying hematologic malignancy. Fortunately, the investigation for an underlying malignancy yielded no results. Early initiation of high-dose intravenous steroids in this patient ultimately led to a favorable outcome, with significant symptom reduction and improved skin findings observed during dermatology follow-up.
Conclusion1,2,3,4
This case involves a patient displaying symptoms of sweet syndrome, a condition characterized by skin alterations and fever. The resemblance to cellulitis often leads physicians to initiate empirical antibiotic treatment. It is crucial to promptly identify this disease, as the appropriate treatment involves steroids, not antibiotics. Providers should be mindful that sweet syndrome is frequently linked to underlying inflammatory conditions and malignancies, underscoring the need for a comprehensive assessment and examination of patients with confirmed or suspected instances of this disease.
References
- Nguyen K R, Lacy A J, Hilbert S, et al. (November 14, 2023) A Not-So-Sweet Syndrome: A Case Report of a Male Presenting with Acute Febrile Neutrophilic Dermatosis. Cureus 15(11): e48810. doi:10.7759/cureus.48810.
- White JM, Mufti GJ, Salisbury JR, du Vivier AW: Cutaneous manifestations of granulocyte colony-stimulating factor. Clinical and Experimental Dermatology. 2006, 31:206-7. 10.1111/j.1365-2230.2005. 01996.x
- Sweet syndrome (neutrophilic dermatosis). (2010). Accessed: 11/4/2023: https://commons.wikimedia.org/wiki/File:Sweet_Syndrome_(neutrophilic_dermatosis)_(4703671002).jpg.
- Von den Driesch P: Sweet’s syndrome (acute febrile neutrophilic dermatosis). Journal of the American Academy of Dermatology. 1994, 31:535-56. 10.1016/s0190-9622(94)70215-2