The clinical presentation of superficial fungal infections varies depending on the infective sites and the specific Candida species involved, posing a significant challenge for diagnosis and treatment in clinical settings without mycological or pathological evidence. The most prevalent forms of superficial candidiasis include oral mucosal candidiasis and onychomycosis. Typically, oral mucosal candidiasis manifests as white or erythematous thrush covering the tongue and other areas within the oral cavity.
Onychomycosis caused by Candida spp. is characterized by thick, fragile, or cracked fingernails or toenails exhibiting yellow or white discoloration. In this report, we present a case of a patient with a black hairy tongue due to Candida tropicalis and another case of greenish-discolored onychomycosis caused by Candida parapsilosis. They conducted a literature search for cases of superficial candidiasis with similar discolored lesions, comparing them with their cases regarding clinical manifestation, causative pathogen, and treatment. These cases underscore the significance of mycological diagnosis in identifying non-Candida albicans Candida species (NCAC) in superficial infections, guiding effective therapeutic approaches.
Superficial Fungal Infections: Introduction
Candida spp. stands out as a leading cause of both superficial and potentially life-threatening systemic fungal infections. Within the spectrum of superficial fungal conditions, notable instances include oral mucosal infections and onychomycosis [1]. Candida albicans continues to be the most prevalent species responsible for superficial infections, aligning with its widespread colonization in mucosal areas [2]. Notably, about half of the healthy individuals carry Candida in their oral cavities in a nonpathogenic yeast state [3]. Factors contributing to the transition from yeast to pathogenic hyphae include broad-spectrum antibiotic therapy, corticosteroids, immune suppression, diabetes mellitus, and nutritional deficiencies [4–6]. However, in the last 10–30 years, non-Candida albicans Candida species (NCAC) have emerged as significant opportunistic human pathogens. Despite C. albicans maintaining its status as the primary causative agent, NCAC species are becoming increasingly prevalent in specific patient populations, especially among neutropenic patients [7,8].
The clinical presentations of superficial candidiasis vary depending on the infectious sites and the specific Candida species involved. This variability poses a significant challenge for diagnosis in clinical settings, particularly when relying solely on clinical presentations [9]. Typically, oral mucosal candidiasis exhibits pseudomembranous thrush, characterized by a white coating or curdish patches on the tongue or other interior areas of the oral cavity [2]. Onychomycosis caused by Candida spp. often manifests as thick, fragile, or cracked fingernails or toenails with yellow or white discoloration, which may not be easily distinguishable from nail infections caused by dermophyte species [10]. In this context, two cases of superficial candidiasis were presented, where patients exhibited green-black changes on the tongue and nails, attributed to non-Candida albicans Candida species.
Superficial Fungal Infections: Case Presentation [1]
Case 1
- Patient History:
- A 50-year-old female was diagnosed with chronic myelogenous leukemia (CML).
- Underwent genotypically matched hematopoietic stem cell transplantation from her brother.
- Hospital Admission:
- Admitted seven months post-transplantation for graft versus host disease (GVHD).
- Oral Symptoms:
- The tongue exhibited black discoloration and a hairy appearance.
- No itch or pain was reported, and no impact on mouth/tongue movements.
- Patient Habits:
- Denies a history of oral hygiene issues and past smoking.

Figure 1: Black hairy tongue on the dorsum of the tongue.
- Physical Examination Findings:
- A greenish-black discolored patch on the tongue with elongated “hair” (3×5 cm) is shown in (Figure 1).
- Surrounded by irregular white pseudomembranous patches.
- Microscopic Examination:
- Specimen taken from discolored area.
- Calcofluor-white fluorescent staining revealed spores and hyphae (Figure 2A).
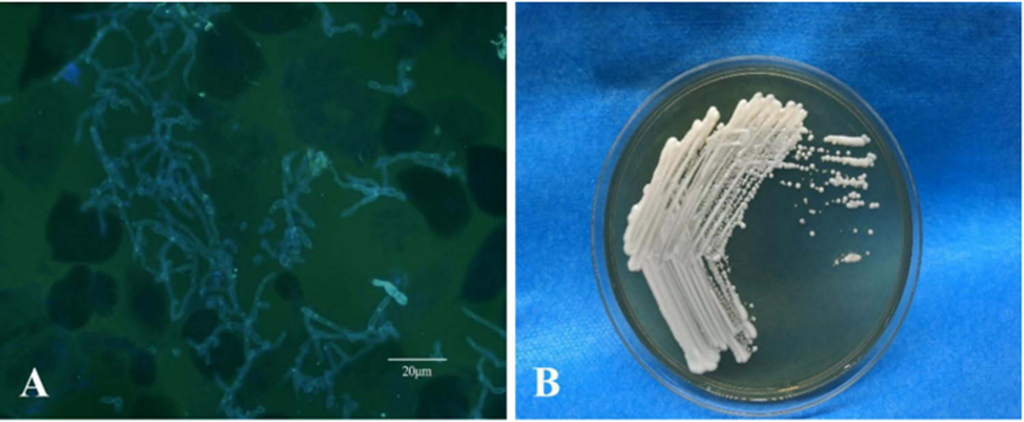
Figure 2: Direct fluorescence microscopy showed blastospores and pseudohyphae (A). On Sabourauds glucose agar at 27°C, cream-colored yeast-like colonies first developed in 3 days (B).
- Microbial Culture:
- Specimens were divided; one portion was stained, and another was inoculated on various media.
- Cream-colored yeast-like colonies appeared on Sabouraud’s Dextrose Agar (SDA) and Potato Dextrose Agar (PDA) by day 3 (Figure 2B).
- Few bacterial colonies, predominantly fungal growth.
- Microbial Identification:
- Fungal species were identified through sequencing internal transcribed spacer (ITS) and beta-tubulin (TB) genes.
- Primer sets used: ITS1 (5′-TCCGTAGGTGAACCTGCGG -3′), ITS4 (5′-TCCTCCGCTTATTGATATGC-3), β-tubulin 2a (5′-AATTGGTGCCGCTTTCTGG-3′) and β-tubulin 2b (5′- AGTTGTCGGGACGGAATAG-3′).
- Sequencing Results:
- Mega blast search in NCBI’s GenBank confirmed the closest relation to Candida tropicalis (GenBank KC422426.1).
- Diagnosis:
- Black hairy tongue attributed to C. tropicalis infection.
- Treatment Initiation:
- Antifungal treatment was initiated promptly post-diagnosis.
- Antifungal Medication:
- Oral itraconazole was administered at 200 mg once daily.
Treatment Outcome:
- Remarkable improvement was observed.
- Black coloration of the tongue resolved within 3 days of treatment.
Case 2
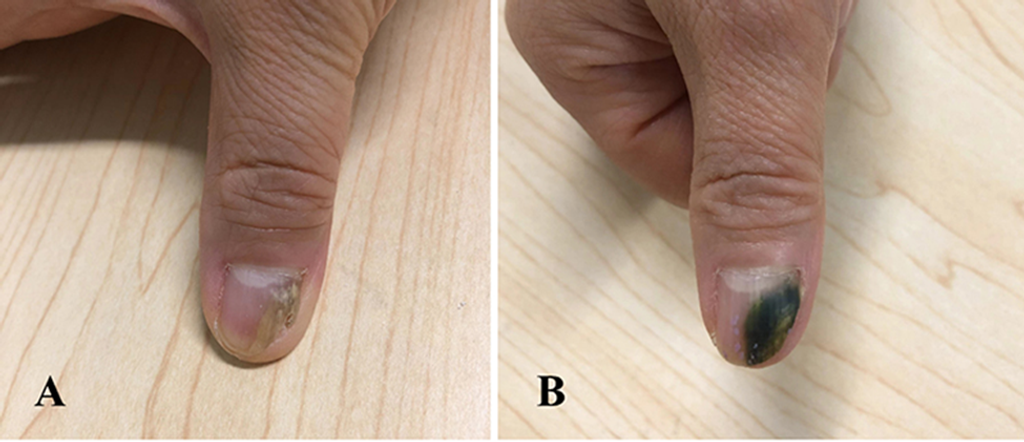
Figure 3: The lesion covered half of the outer edge of the nail plate with yellowish discoloration (A), after 3 months of therapy, and her thumbnail presented with green-black discoloration (B).
- Patient Presentation:
- A 52-year-old woman sought consultation at the Dermatology Department with a primary concern of thickening and discoloration.
- Affected areas included the right thumbnail, big and little toenails on the right foot, and the middle and little toenails on the left foot for a 5-month duration (Figure 3A).
- Medical History:
- No significant past medical conditions or history of drug use.
- No nail trauma preceding the onset of the infection.
- Initial Treatment:
- Empirical treatment with oral itraconazole: 200 mg twice daily for one week, followed by a 3-week interruption in each 4-week cycle.
- Progress and Changes:
- Significant improvement was observed in toenails after months of treatment.
- The thumbnail showed no improvement but increased size and greenish-black hue, as shown in (Figure 3B).
- Distal onycholysis was observed on the inferior surface of the discolored thumbnail.
- Microscopic Examination:
- Sub-spherical budding yeast-like cells were found in the specimen from the right thumbnail (Figure 4A).
- Mycelium was observed on affected toenails.
- Initial diagnosis: Onychomycosis caused by dermatophytes.
- Laboratory Tests:
- No abnormality in blood works.
- The affected right thumbnail observed diffuse green discoloration, proximal nail fold involvement, and distal onycholysis.
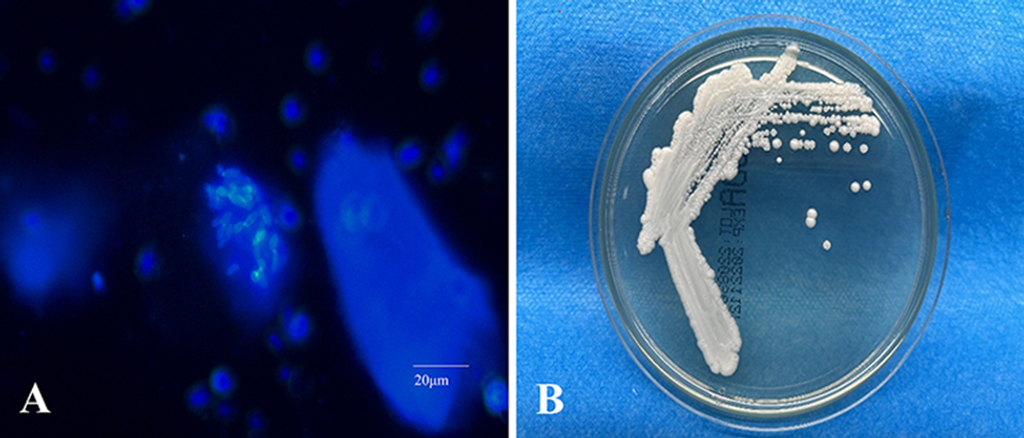
Figure 4: Microscopic examination revealed sub-spherical budding yeast-like cells without pseudohyphae structure (A); Three days later, at 27°C, creamy yeast-like colonies appeared on the SDA plate (B).
- Cultural Analysis:
- Specimen cultured on BA and SDA plates at 27°C.
- The bacterial culture on BA was negative after 3 days.
- Repeated microscopic examination and cultures consistently identified the same yeast-like colony appearance (Figure 4A).
- The repeated cultures yielded the same yeast-like colony appearance (Figure 4B).
- Identification of Causative Agent:
- Morphological features and molecular sequencing confirmed C. parapsilosis as the causative agent in the right thumbnail infection.
- Antifungal Susceptibility Testing:
- Performed according to Clinical and Laboratory Standards Institute M27-A3 protocol.
- The broth microdilution method was used to test eight agents against the isolated strain.
- MIC values: Itraconazole (1.0 μg/mL), voriconazole (0.125 μg/mL), amphotericin B (1.0 μg/mL), posaconazole (0.25 μg/mL), nystatin (4.0 μg/mL), micafungin (1.0 μg/mL), fluconazole (1.0 μg/mL), terbinafine (>0.5 μg/mL).
- Treatment Adjustment:
- Changed to oral fluconazole 150 mg weekly for 3 months.
- Nail discoloration faded, and no signs of relapse were noted at the one-month follow-up.
Superficial Fungal Infections: Discussion
We present a case involving a black hairy tongue induced by C. tropicalis in an immunocompromised patient and another case of onychomycosis caused by C. parapsilosis in a patient with no underlying health issues. Both instances exhibit greenish-black lesions and demonstrate favorable responses to azole antifungal treatment [1]. Greenish-black discoloration from Candida spp. is less prevalent in oral and skin fungal infections than pigment-producing bacterial and fungal pathogens like Aspergillus spp. and Pseudomonas spp.
Black hairy tongue (BHT) is identifiable by its distinct black hue, as illustrated in Case 1. In this particular case, a painless black, hair-like lesion appeared on the dorsum of the tongue, anterior to the circumvallate papillae. BHT is a harmless medical condition characterized by elongated filiform lingual papillae, presenting a carpet-like appearance on the dorsum of the tongue. The infected tongue’s hairy surface may exhibit discoloration ranging from blackish-brown to yellowish-green or an unpigmented color [6]. In cases of BHT caused by Candida spp., primary manifestations include the loss of papillae on the dorsal tongue, erythematous patches, fissuring of the tongue, and potential extension to other mucosal surfaces or the corners of the mouth (angular cheilitis) [13]. Generally, BHT does not manifest on the tip or sides of the tongue. Differential diagnosis for BHT encompasses various bacterial and fungal infections, with no distinctive symptoms indicating a fungal origin [14].
A review of the medical literature indicates that Black Hairy Tongue (BHT) is not uncommon, with incidence rates ranging from 0.6% to 18% in different study populations. The etiology of BHT remains unclear and is likely multifactorial, resulting from a combination of local and systemic insults. Numerous noninfectious predisposing factors are associated with BHT-like manifestations, including smoking, exposure to irritants leading to poor oral hygiene, and conditions such as acanthosis nigricans and oral hairy leukoplakia [16,17]. Previous clinical observations have linked heavy tobacco use to an increased risk of BHT.
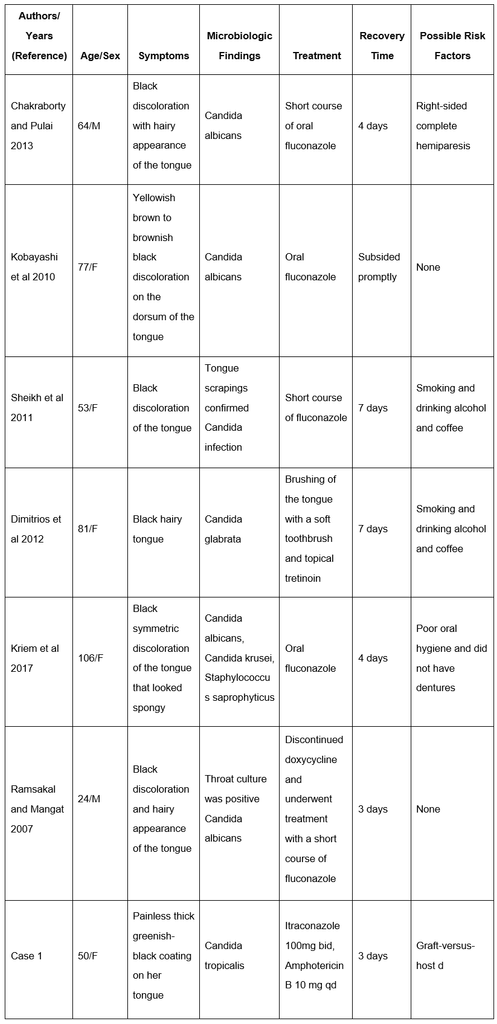
A comprehensive search of online databases, such as PubMed and Web of Science, was conducted, and the reference lists of all retrieved articles, including review articles, were examined. The search spanned from 2000 to 2022, using terms like “black hairy tongue,” “black tongue,” “hyperpigmented tongue,” “lingua villosa nigra,” and “hairy tongue.” In total, our literature search identified six cases of Candida-related BHT. Table 1 outlines the clinical characteristics of patients with Candida-related BHT. Among the six patients, two were male, and four were female, with ages ranging from 3 months to 106 years old. Four patients with poor oral hygiene exhibited one or more risk factors for BHT, including smoking, alcohol and coffee consumption, and edentulism. Mycological identification revealed that none of them were caused by Candida tropicalis. All six patients responded well to antifungal therapy, fully recovering from BHT through good oral hygiene.
Utilizing systemic and local medications can induce or worsen Black Hairy Tongue (BHT). Antibiotics, including linezolid, penicillin, and erythromycin, have been linked to this disorder, although the precise mechanisms leading to black hairy tongue in association with antibiotics remain unclear [19]. Antibiotic use could alter the oral microbiota. Additionally, significant anatomical changes in the filiform papillae may predispose patients to trap foreign material or promote microbial overgrowth, resulting in the characteristic color change seen in BHT patients. One potentially implicated bacterium is Porphyromonas gingivalis, a black-pigmented gram-negative anaerobic rod known for its role in chronic periodontitis. Still, this theory is speculative and does not account for cases with different discolorations [18,20].
While Candida tropicalis can be found in oral cavities, the specific mechanism connecting microflora such as C. tropicalis to the greenish-black discoloration in BHT is unclear. Onychomycosis, characterized by nail discoloration ranging from white to yellow to brown, presents clinically with symptoms such as onycholysis, brittleness, nail thickening, and subungual accumulation of scale. In Case 2, caused by C. parapsilosis, an atypical coloration was observed in the right thumbnail, and although previous studies reported dark discoloration by C. parapsilosis, the exact mechanism remains uncertain [15,17].
A literature review from 2000 to 2022 identified cases showing green or black skin and nail lesions caused by Candida spp., similar to Case 2. Fungal melanonychia, a rare nail disorder with longitudinal dark pigmentation, was associated with Candida albicans and non-Candida albicans Candida (NCAC).
The term “viridionychia” has been introduced to describe fungal etiology-associated green nail syndrome, and it is particularly linked to Candida parapsilosis [5,18].
Differentiating green nail syndrome from bacterial infections, such as Pseudomonas aeruginosa, is crucial. P. aeruginosa produces pigmented virulence factors, giving green nail syndrome, also known as Goldman–Fox syndrome, a characteristic blue-green color. Fungal-associated green nail syndrome is less common than bacterial origins, possibly due to P. aeruginosa inhibiting fungal growth. Nail dermoscopy has been suggested for identifying mixed infections.
In Case 2, the discolored thumbnail responded to fluconazole after itraconazole failed. Non-itraconazole responsiveness suggests a possible mixture of Candida spp. in the thumbnail. Individual nail specimen collection may be necessary, especially when nail treatment responses differ. When C. parapsilosis is identified, oral treatment with terbinafine or fluconazole, combined with topical application of amphotericin B, is recommended based on susceptibility tests indicating sensitivity to these drugs.
Conclusion
In conclusion, as the study and other sources documented, the investigation revealed a noticeable greenish-black discoloration associated with superficial candidiasis caused by both C. tropicalis and C. parapsilosis. While immunosuppressive therapy and nail damage emerged as potential risk factors in our two cases, the specific fungal or host agents responsible for the greenish-black discoloration remain unidentified, suggesting a multifactorial origin. Establishing a correlation between Candida species and this discoloration proved challenging, given the rarity of fungal-associated Black Hairy Tongue (BHT) and green nail syndrome.
References
- Shi L, Feng Y, Shi D. Two Cases of Superficial Fungal Infection Caused by Non-Albicans Candida Species Manifest Greenish-black Discoloration. Infect Drug Resist. 2024;17:665-672 https://doi.org/10.2147/IDR.S438079.
- Latgé JP, Calderone R. Host-microbe interactions: fungi invasive human fungal opportunistic infections. Curr Opin Microbiol. 2002;5(4):355–358.doi:10.1016/S1369-5274(02)00343-0
- Millsop JW, Fazel N. Oral candidiasis. Clin Dermatol. 2016;34(4):487–494. doi: 10.1016/j.clindermatol.2016.02.022
- Arendorf TM, Walker DM. The prevalence and intra-oral distribution of Candida albicans in man. Arch Oral Biol. 1980;25(1):1–10. doi:10.1016/0003-9969(80)90147-8
- Warrier SA, Sathasivasubramanian S. Human immunodeficiency virus induced oral candidiasis. J Pharm Bioallied Sci. 2015;7(Suppl 2): S812–S814. doi:10.4103/0975-7406.163577
- Shetti A, Gupta I, Charantimath SM. Oral candidiasis: aiding in the diagnosis of HIV-A case report. Case Rep Dent. 2011; 2011:929616. doi:10.1155/2011/929616
- Gurvits GE, Tan A. Black hairy tongue syndrome. World J Gastroenterol. 2014;20(31):10845–10850. doi:10.3748/wjg. v20.i31.10845.
- Nucci M, Colombo AL. Candidemia due to Candida tropicalis: clinical, epidemiologic, and microbiologic characteristics of 188 episodes occurring in tertiary care hospitals. Diagn Microbiol Infect Dis. 2007;58(1):77–82. doi: 10.1016/j.diagmicrobio.2006.11.009
- Silva S, Negri M, Henriques M, Oliveira R, Williams DW, Azeredo J. Candida glabrata, Candida parapsilosis and Candida tropicalis: biology, epidemiology, pathogenicity and antifungal resistance. FEMS Microbiol Rev. 2012;36(2):288–305. doi:10.1111/j.1574-6976.2011. 00278.x
- Hay RJ, Baran R, Moore MK, Wilkinson JD. Candida onychomycosis–an evaluation of the role of Candida species in nail disease. Br J Dermatol.1988;118(1):47–58. doi:10.1111/j.1365-2133. 1988.tb01749.x
- Lipner SR, Scher RK. Onychomycosis: treatment and prevention of recurrence. J Am Acad Dermatol. 2019;80(4):853–867. doi:10.1016/j. jaad.2018.05.1260
- Korabecná M, Liska V, Fajfrlík K. Primers ITS1, ITS2, and ITS4 detect the intraspecies variability in the internal transcribed spacers and 5.8SrRNA gene region in clinical isolates of fungi. Folia Microbiol. 2003;48(2):233–238. doi:10.1007/BF02930961.
- Wayne P. Clinical and Laboratory Standards Institute: Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; Approved Standard; CLSI Document M27-A3. Clinical and Laboratory Standards Institute; 2008.
- Hu L, He C, Zhao C, Chen X, Hua H, Yan Z. Characterization of oral candidiasis and the Candida species profile in patients with oral mucosal diseases. Microb Pathog. 2019; 134:103575. doi: 10.1016/j.micpath.2019.103575.
- McGrath EE, Bardsley P, Basran G. Black hairy tongue: what is your call. CMAJ. 2008;178(9):1137–1138. doi:10.1503/cmaj.071611.
- Redman RS. Prevalence of geographic tongue, fissured tongue, median rhomboid glossitis, and hairy tongue among 3611 Minnesota schoolchildren. Oral Surg Oral Med Oral Pathol. 1970;30(3):390–395. doi:10.1016/0030-4220(70)90320-8.
- Avcu N, Kanli A. The prevalence of tongue lesions in 5150 Turkish dental outpatients. Oral Dis. 2003;9(4):188–195. doi:10.1034/j.1601-0825.2003. 02933.x
- Korber A, Dissemond J. Images in clinical medicine. Black hairy tongue. N Engl J Med. 2006;354(1):67. doi:10.1056/NEJMicm050117.
- Guhl G, Díaz Ley B. Lengua negra vellosa [Black hairy tongue]. Med Clin. 2011;137(4):192. Spanish. doi: 10.1016/j.medcli.2010.01.022.
- Chakraborty PP, Pulai D. Black hairy tongue (lingua villosa nigra). J Assoc Physicians India. 2013;61(12):908.
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!






