Spontaneous Hemoperitoneum in pregnancy (SHiP) is a rare but life-threatening condition for both mother and baby. Though it can strike at any stage of pregnancy, it’s most commonly seen in the third trimester. The exact cause of SHiP remains a mystery. Still, endometriosis and adenomyosis are significant risk factors, often leading to ruptures in the utero-ovarian vasculature or bleeding from endometrial foci in the abdomen. Here, we spotlight a rare case of a pregnant patient in her third trimester experiencing a uterine adenomyosis rupture and bleeding from endometrial foci.
Introduction: Spontaneous Hemoperitoneum and Adenomyosis
Spontaneous haemoperitoneum in pregnancy (SHiP) may be rare, but it’s a critical condition that demands attention from gynecologists and obstetricians. This spontaneous, non-traumatic intraperitoneal hemorrhage can occur during pregnancy or up to 42 days postpartum, posing numerous serious obstetric complications [1,2].
Though SHiP can strike at any time, it most frequently occurs in the third trimester, manifesting as acute abdominal pain and often requiring urgent surgical intervention [3].
Adenomyosis, a benign disorder where endometrial tissue infiltrates the myometrium, is strongly linked to adverse perinatal outcomes. Women with adenomyosis face higher risks of preterm delivery, preeclampsia (PE), cesarean delivery, postpartum hemorrhage, and delivering small-for-gestational-age infants [4].
Content Warning: This article contains explicit medical imagery. Viewer discretion is advised.
Case Presentation
- Patient Profile: 36-year-old primipara, conceived spontaneously, with gestational diabetes managed by diet.
- Emergency Admission: Presented at the Department of Gynaecology, University Medical Centre Ljubljana, Slovenia, for acute abdomen at 26 weeks and three days of gestation.
- Initial Presentation: Admitted to a peripheral hospital hour earlier due to sudden severe abdominal pain.
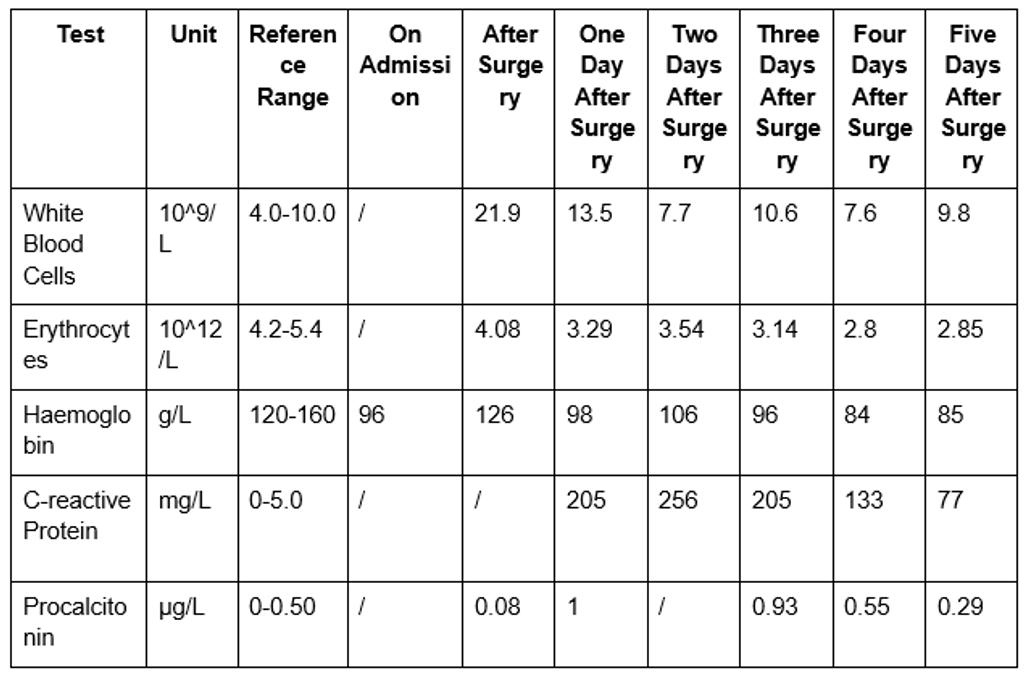
- Lab Results: Initial tests showed haemoglobin levels at 96 g/l (Table 1).
- Ultrasound Findings:
- Viable fetus with a heartbeat
- Adequate amniotic fluid
- Anterior placenta extending beyond the internal uterine orifice
- No evidence of retroplacental hematoma
- Vaginal Examination:
- Shortened, closed cervix
- No discharge (Bishop’s score: 3)
- Cardiotocograph: Normal results
- Treatment: Spasm analgesic therapy administered:
- Trospium chloride: 0.2 mg
- Metamizole: 2.5 g
Table 1: Laboratory values before and after the surgery
- Normal Pregnancy: Until 26 weeks and three days.
- Medical History:
- Three spontaneous pneumothoraces of unknown cause in the year before conception.
- Large loop excision of the transformation zone (LLETZ) for a cervical lesion.
- No other medical conditions.
- Emergency Situation:
- Abdominal ultrasound showed a large amount of free fluid in the abdominal cavity and a viable pregnancy with no signs of labor.
- The abdomen was tense and painful on palpation.
- The patient developed hemorrhagic shock and was immediately transferred to the operating theatre.
- Surgical Team: Gynecological surgeon, obstetrician assistant, neonatologist, and abdominal surgeon (due to suspected hollow organ perforation).
- Surgical Findings:
- Upon entering the abdominal cavity via a midline incision, approximately one liter of blood and clots were found.
- Gastrointestinal and vascular causes of bleeding were excluded.
- A 5 cm bleeding ulcer was found on the uterus under the round ligament and a ruptured left parametrium (Figure 1).
- Emergency C-Section:
- Performed due to the life-threatening condition of the patient and fetus.
- Delivered a breech-presenting female newborn weighing 820 g with an Apgar score of 3/6.
- Intact placenta observed.
- No communication was found between the uterine cavity and the lesion.
- Post-Delivery Procedures:
- Uterine exploration and suturing with a running suture.
- Abdominal hysterectomy without adnexa due to uncontrollable massive bleeding.
- Estimated blood loss: 2200 ml.
- Received 1190 ml (four units) of blood group 0 positive erythrocyte transfusion.
- Recovery:
- The patient recovered without complications.
- Discharged to home care on the ninth postoperative day.
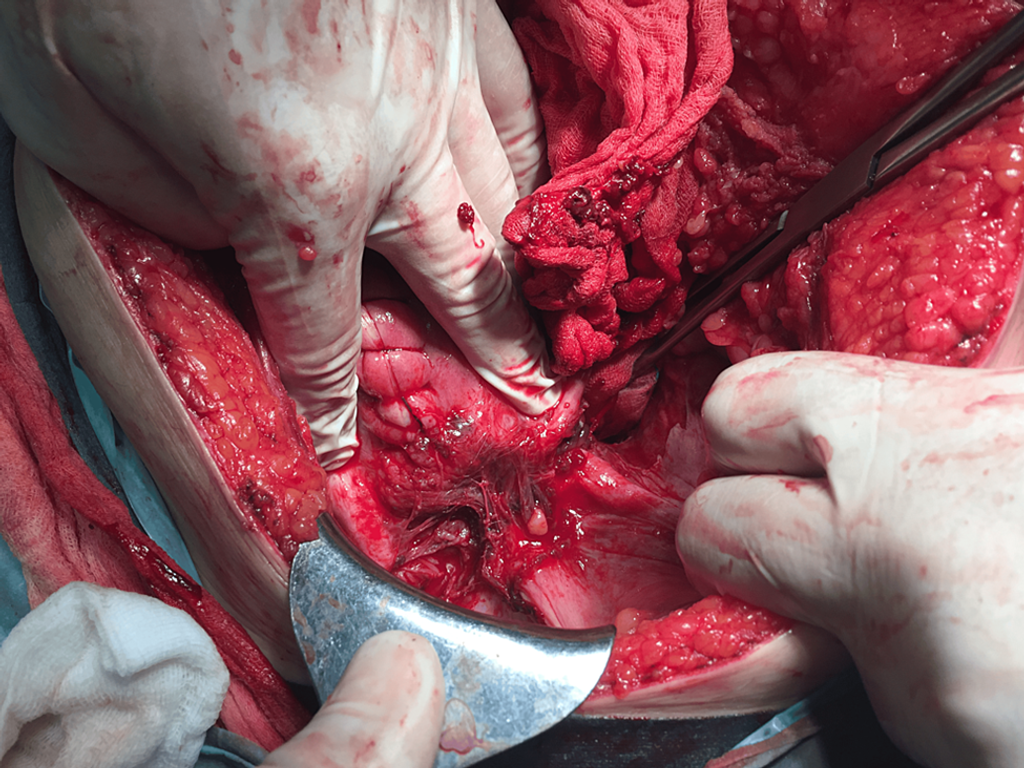
Figure 1: A large bleeding ulcer on the uterus to the left from the plica vesica uterine
- Diagnosis: Uterine histology revealed adenomyosis with multiple, large foci overgrowing the serosa (Figure 2).
- Foci Location: Predominantly in the subserosal myometrial area.
- Additional Findings:
- Abundant decidualized endometriotic foci in tissue samples from the uterine vesical fold.
- Endometriotic foci also present in the peritoneum of the sigmoid colon.
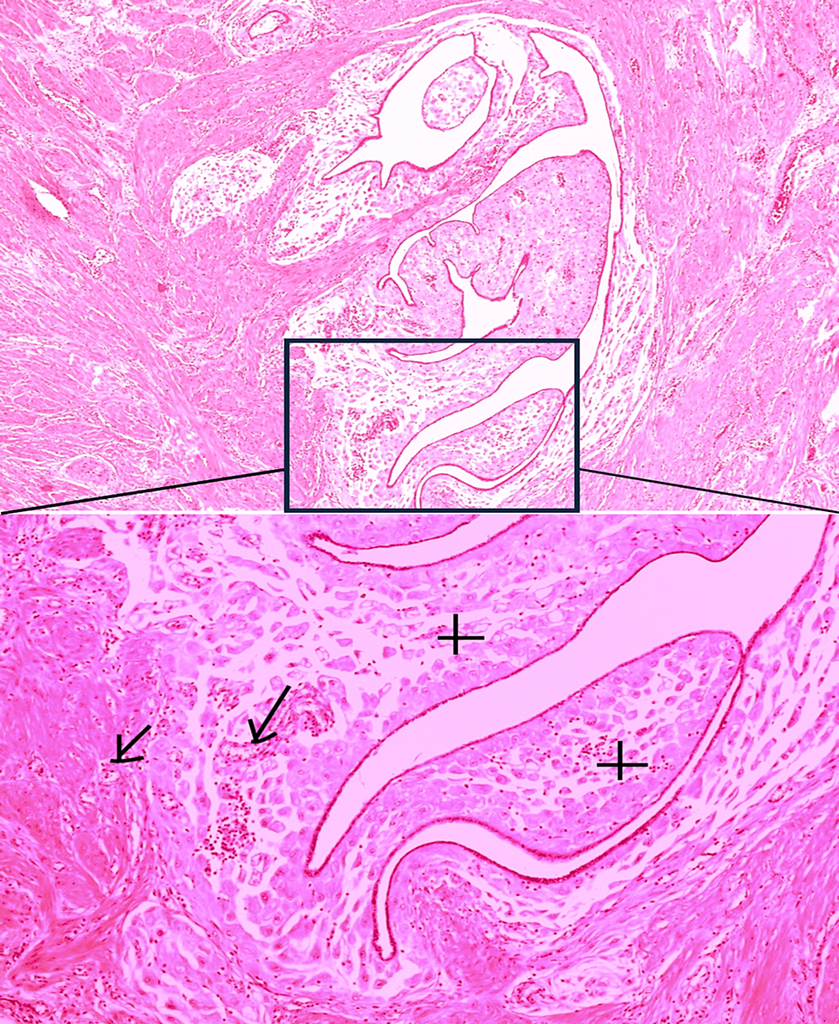
Figure 2: Decidual reaction of adenomyosis, which led to a uterine rupture
- Initial Challenges:
- Birth: Newborn was not breathing.
- Oxygen Saturation: Below 60% despite 100% oxygen mask ventilation.
- Intubation: Performed three minutes after birth.
- NICU Transfer: To Ljubljana Maternity Hospital with positive pressure ventilation.
- Immediate Treatment:
- Surfactant Replacement: Administered upon NICU admission, reducing oxygen and ventilatory support needs.
- Ventilatory Support:
- Duration: 23 days of synchronized intermittent positive-pressure ventilation.
- Subsequent Support: 19 days of non-invasive mask ventilation.
- Supplemental Oxygen: Provided via nasal tubes for adequate oxygenation.
- Complications and Treatments:
- Hospital-Acquired Pneumonia: Treated with flucloxacillin for Staphylococcus aureus infection.
- Patent Ductus Arteriosus: Closed with two courses of indomethacin.
- Anemia: Required early red blood cell transfusion (day 12) and recombinant human erythropoietin to stimulate erythropoiesis.
- Health Monitoring and Outcomes:
- Perinatal Asphyxia: Despite metabolic acidosis (pH 7.09, BE 12.2), no cerebral hemorrhage or asphyxia on ultrasound.
- Neurological Status: Normal for gestation at discharge.
- Retinopathy of Prematurity: Diagnosed at 53 days (34 weeks postmenstrual age) and regressed by discharge.
- Discharge and Follow-Up:
- Age at Discharge: 72 days (37 weeks postmenstrual age), weighing 2600 g, still requiring supplemental oxygen for chronic lung disease of immaturity.
- Outpatient Follow-Up: Continued until two years corrected age.
- Oxygen Supplementation: Discontinued three months after discharge.
- Development: Initially mild delay in gross motor skills; caught up with peers in growth and development by last check-up.
Discussion
We present a rare case of haemoperitoneum in pregnancy caused by adenomyosis, manifesting as acute abdominal pain in the third trimester. This condition resulted in significant intra-abdominal hemorrhage, necessitating immediate surgical intervention, including an emergency cesarean section followed by a hysterectomy to control the bleeding.
The literature identifies endometriosis and ovarian hyperstimulation during assisted reproductive technology (ART), such as IVF, as significant risk factors for SHiP [3,5]. Pregnancies achieved through ART and complicated by endometriosis exhibit a higher incidence and severity of SHiP compared to spontaneous pregnancies with endometriosis [5]. A recent study by Mazzocco et al. reported that 0.3% of 362 pregnant women with endometriosis who conceived via ART developed SHiP [6].
Conclusions
The case underscores the urgency of swiftly recognizing and managing SHiP, a rare but life-threatening condition. With endometriosis as a major risk factor, understanding its underlying mechanisms is crucial for effective treatment. Our discovery of uterine adenomyosis as a rare cause highlights the complexity of SHiP’s origins. Despite the challenges in identifying the issue during surgery, our case illustrates the necessity of rapid surgical intervention to reduce risks for both mother and baby. Ongoing research is essential to unravel SHiP’s multifaceted causes and enhance clinical strategies, ultimately improving outcomes for pregnant women and their infants.
References
- Krajec M, Lebar V, Kornhauser Cerar L, et al. (July 02, 2024) Spontaneous Haemoperitoneum in the Third Trimester of Pregnancy Due to Adenomyosis: A Case Report. Cureus 16(7): e63718. doi:10.7759/cureus.63718
- Kapila P: Fatal non-traumatic spontaneous hemoperitoneum in second trimester of pregnancy–autopsy findings. J Forensic Leg Med. 2011, 18:139-40. 10.1016/j.jflm.2011.01.012
- Lier MC, Malik RF, Ket JC, Lambalk CB, Brosens IA, Mijatovic V: Spontaneous hemoperitoneum in pregnancy (SHiP) and endometriosis – a systematic review of the recent literature. Eur J Obstet Gynecol Reprod Biol. 2017, 219:57-65. 10.1016/j.ejogrb.2017.10.012
- Brosens IA, Fusi L, Brosens JJ: Endometriosis is a risk factor for spontaneous hemoperitoneum during pregnancy. Fertil Steril. 2009, 92:1243-5. 10.1016/j.fertnstert.2009.03.091
- Sayama S, Iriyama T, Takeiri Y, et al.: Clinical characteristics and outcomes of women with adenomyosis pain during pregnancy: a retrospective study. J Perinat Med. 2024, 52:186-91. 10.1515/jpm-2023-0263
- Brosens IA, Lier MC, Mijatovic V, Habiba M, Benagiano G: Severe spontaneous hemoperitoneum in pregnancy may be linked to in vitro fertilization in patients with endometriosis: a systematic review. Fertil Steril. 2016, 106:692-703. 10.1016/j.fertnstert.2016.05.025
- Mazzocco MI, Donati S, Maraschini A, Corsi E, Colciago E, Guelfi F, Cetin I: Spontaneous hemoperitoneum in pregnancy: Italian prospective population-based cohort study. Acta Obstet Gynecol Scand. 2022, 101:1220-6. 10.1111/aogs.14431
- Brosens JJ, Gellersen B: Death or survival–progesterone-dependent cell fate decisions in the human endometrial stroma. J Mol Endocrinol. 2006, 36:389-98. 10.1677/jme.1.02060
- O’Leary SM: Ectopic decidualization causing massive postpartum intraperitoneal hemorrhage. Obstet Gynecol. 2006, 108:776-9. 10.1097/01.AOG.0000200596. 98039.c5
- Katorza E, Soriano D, Stockheim D, et al.: Severe intraabdominal bleeding caused by endometriotic lesions during the third trimester of pregnancy. Am J Obstet Gynecol. 2007, 197: 501.e1-4. 10.1016/j.ajog.2007.04.030
- Mizumoto Y, Furuya K, Kikuchi Y, Aida S, Hyakutake K, Tamai S, Nagata I: Spontaneous rupture of the uterine vessels in a pregnancy complicated by endometriosis. Acta Obstet Gynecol Scand. 1996, 75:860-2. 10.3109/00016349609054718
- Aziz U, Kulkarni A, Lazic D, Cullimore JE: Spontaneous rupture of the uterine vessels in pregnancy. Obstet Gynecol. 2004, 103:1089-91. 10.1097/01.AOG.0000121833. 79081.c7
- Foley MR, Sonek JD, Lavender LM, Zuspan FP: Spontaneous rupture of uteroovarian veins in pregnancy: two case reports. Am J Obstet Gynecol. 1987, 156:962-4. 10.1016/0002-9378(87)90367-x
- Choobun T, Pinjaroen S, Getpook C: Spontaneous intra-abdominal bleeding during pregnancy. J Med Assoc Thai. 2006, 89:1044-6.
- Steinberg LH, Goodfellow C, Rankin L: Spontaneous rupture of the uterine artery in pregnancy. Br J Obstet Gynaecol. 1993, 100:184. 10.1111/j.1471-0528. 1993.tb15220.x
- Kato M, Miyazaki Y, Kawamura H, Orisaka M, Kurokawa T, Yoshida Y: A 41-year-old woman with spontaneous hemoperitoneum in pregnancy at 28 weeks. Am J Case Rep. 2023, 24: e939330. 10.12659/AJCR.939330
- Vuong AD, Pham TH, Nguyen XT, Trinh NB, Nguyen PN, Ho QN: Spontaneous hemoperitoneum in the second and third trimester of pregnancy: two uncommon case reports at Tu Du Hospital, in Vietnam and a literature review. Int J Emerg Med. 2023, 16:26. 10.1186/s12245-023-00498-w
- Passos F, Calhaz-Jorge C, Graça LM: Endometriosis is a possible risk factor for spontaneous hemoperitoneum in the third trimester of pregnancy. Fertil Steril. 2008, 89:251-2. 10.1016/j.fertnstert.2007.02.009
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!







