The recreational use of methamphetamines is skyrocketing worldwide. This potent stimulant not only poses severe health risks but also has a highly addictive nature, often leading to psychiatric disorders. Alarmingly, suicidal thoughts and attempts are rampant among methamphetamine users, now a leading cause of death alongside accidental overdoses. In this report, we delve into a harrowing case of a methamphetamine user who attempted suicide by jumping off a bridge. We also explore recent research highlighting the chilling link between methamphetamine use and suicide.
Introduction to Methamphetamine
Methamphetamine (MA) use is a growing global crisis, second only to marijuana in terms of prevalence. This powerful stimulant poses severe health risks, with overdoses often proving fatal [1,2]. The danger is compounded by the frequent abuse of other substances like marijuana, alcohol, and opiates alongside MA [3].
MA users face a host of mental and behavioral issues, including anxiety, depression, suicidal ideation, and psychosis. These conditions significantly elevate the suicide risk among MA users [3,4]. Shockingly, injection MA use increases the likelihood of a suicide attempt by 80% compared to non-MA users [5]. Research has shown that a quarter of those who completed MA-related suicides had previously attempted suicide [6]. In the US, hospital admissions for suicidal ideation among MA-dependent individuals have surged 16-fold from 2008 to 2019 [7].
MA use is more prevalent among men, with additional risk factors including HIV/AIDS, criminal justice involvement, and lower household income. However, young women under 25 with psychiatric comorbidities are particularly vulnerable to suicide within the MA user population [2]. These women are also more likely to seek medical help for suicidal thoughts. Notably, MA users with bipolar disorder have the highest suicide risk, followed by those with depression, schizophrenia, and anxiety disorders [8,9].
This study delves into a harrowing case of a young man with a history of MA use who attempted suicide by jumping off a bridge. His story serves as a stark reminder of the grave suicide risks faced by individuals with MA use disorder and underscores the urgent need for comprehensive mental health support.
Case Presentation
Patient Profile
- Demographics: 30-year-old single, unemployed male.
- Incident: Presented to the emergency department after jumping off a 30-foot bridge.
- Consciousness: The patient was conscious upon arrival.
Injuries Sustained
- Fractures:
- Sacral vertebrae
- Pubic rami
- Several ribs (Figure 1)
- Transverse and spinous processes of the lumbar vertebra (Figure 4)
- Hematoma:
- Traumatic retroperitoneal hematoma (Figure 3).
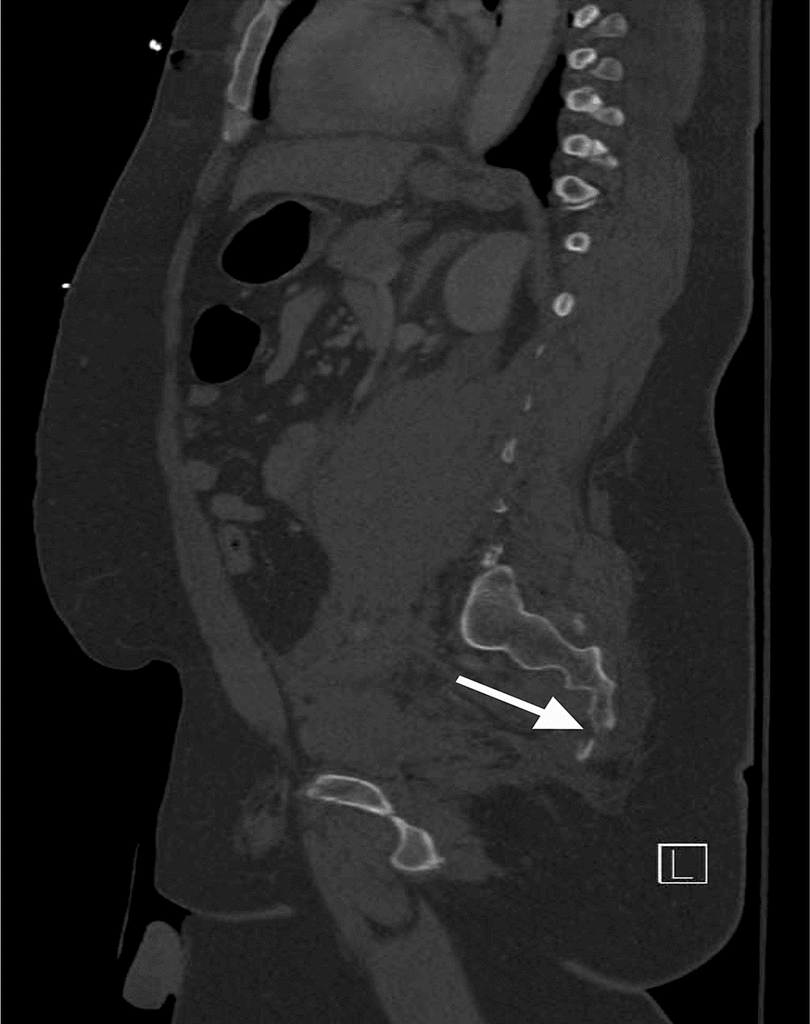
Figure 1: A CT scan of the pelvis shows a distal sacral fracture.
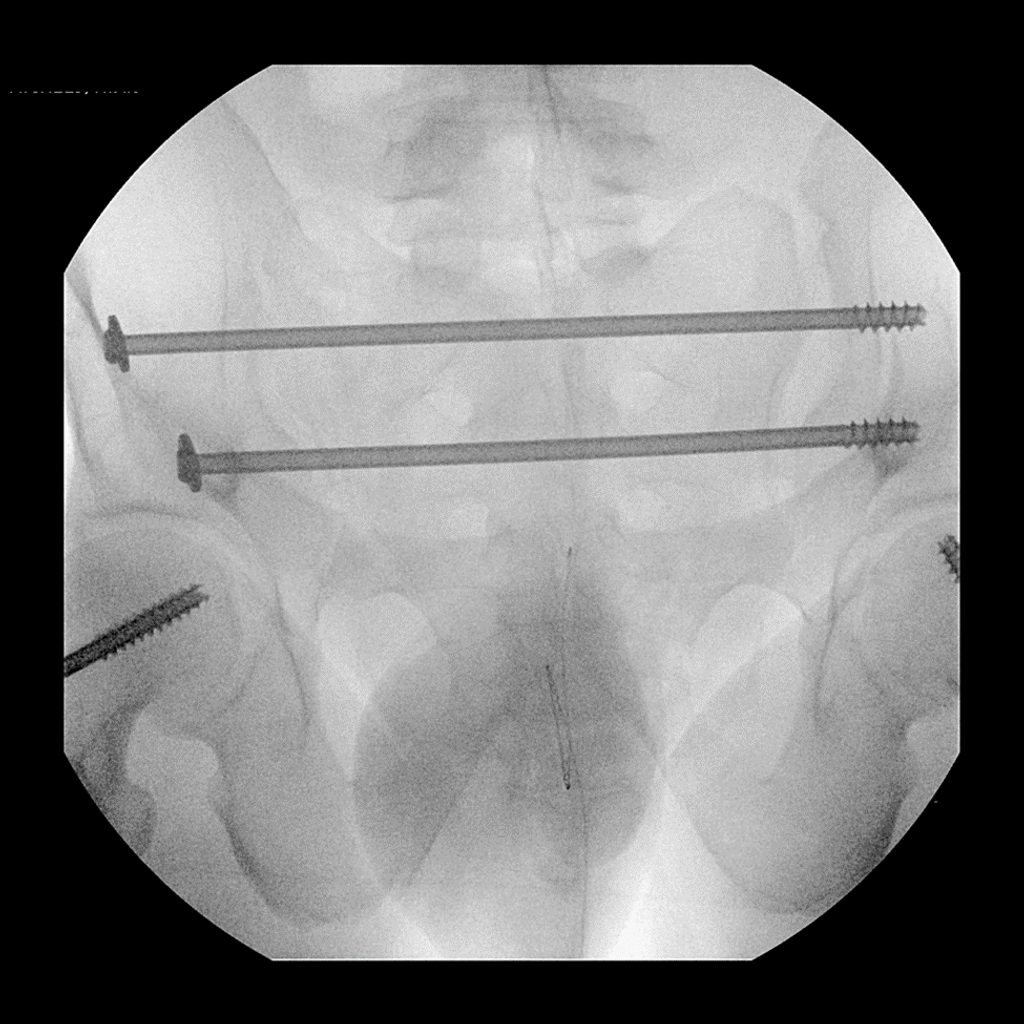
Figure 2: CT scan of the pelvis shows an ORIF of the fracture through the sacroiliac joint with postoperative anatomic alignment.
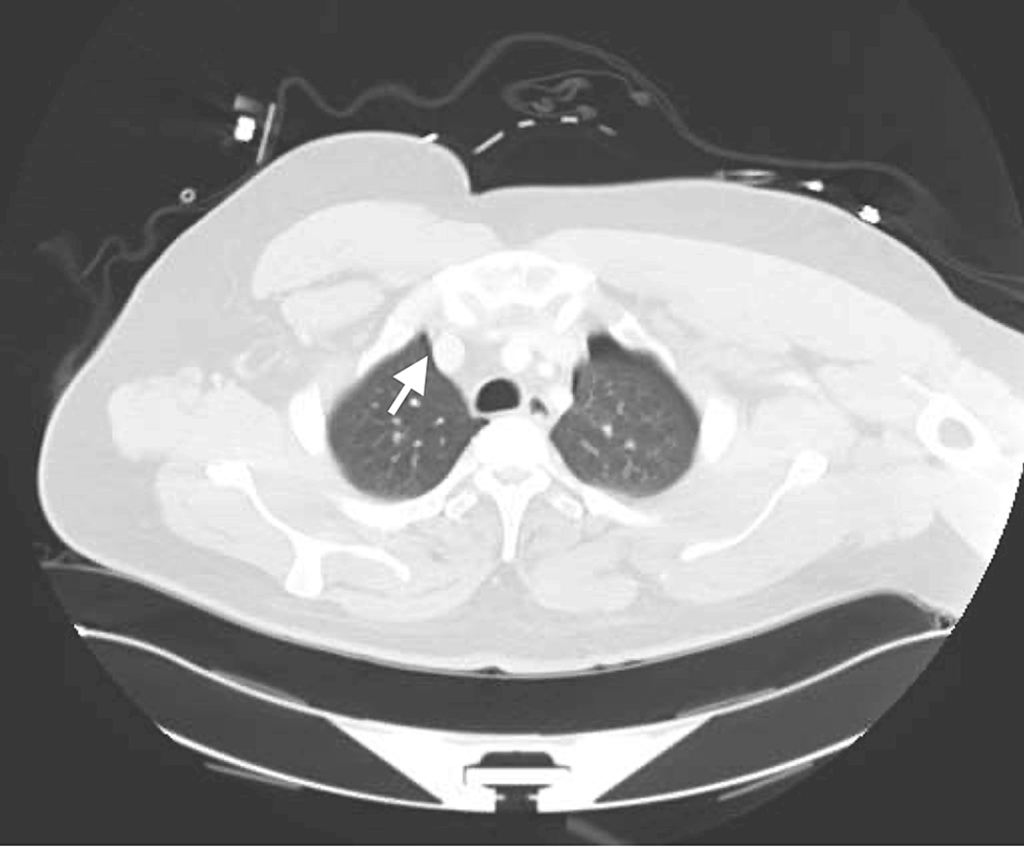
Figure 3: A CT scan of the abdomen shows a left retroperitoneal hemorrhage.
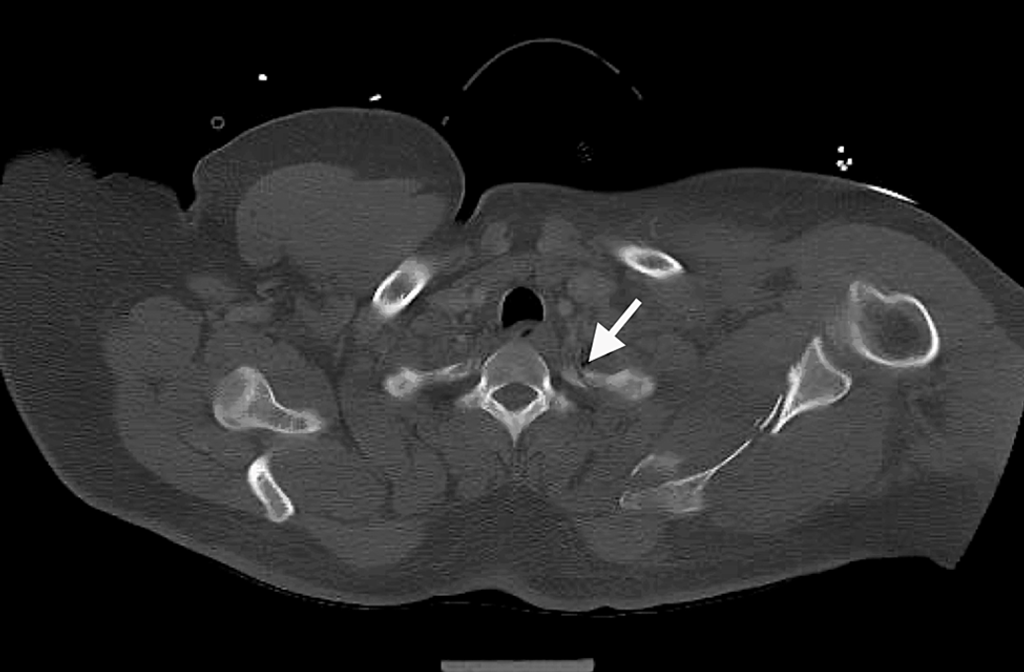
Figure 4: A CT scan of the abdomen shows a fracture of the transverse process of the lumbar spine.
Postoperative Outcomes
- Surgical Intervention: Open reduction and internal fixation.
- Improvement: The sacroiliac joint showed improved anatomic alignment post-surgery (Figure 2).
Psychological and Behavioral Findings
- Mental Health Disclosure: The patient disclosed that the jump was a planned suicide attempt.
- Reported Issues: Severe depression is linked to the inability to control methamphetamine (MA) use and family conflicts.
- Symptoms:
- Sad mood, mood swings, irritability, poor impulse control
- Sleeping disturbances, anhedonia, isolative behaviors, social withdrawal
- Active suicidal ideations
Substance Use and Cognitive Status
- Substance Use: Admitted to consuming “ice” (crystal meth) before the incident.
- Cognitive and Behavioral Observations:
- Initially, he only provided his first name and claimed not to remember his last name.
- Denied his full name even after identification by hospital staff.
- Displayed signs of being “hyped up,” paranoid, and internally preoccupied.
- Denied experiencing hallucinations.
- Restless but not aggressive.
Medical Findings and History
- Patient’s Claim: No significant medical issues.
- Lab Results:
- Leukocytosis and hyperglycemia (Tables 1, 2).
- Positive toxicology screen for amphetamines.
- Psychiatric History:
- Several inpatient psychiatric admissions.
- Diagnosed with depressive disorder and MA use disorder.
- Recently discharged from an inpatient facility days before the incident.
- Previous Suicide Attempts:
- Cutting his arm multiple times.
- Attempted hanging.
- Current Status:
- No current medical or psychiatric provider.
- Noncompliant with psychiatric medications.
- Lost to psychiatric follow-up since discharge.
- Substance Use: Long history of MA use.
- Living Situation: On Disability, living with a sibling.
Medical Management
- Pain Management Medications:
- Acetaminophen, lidocaine, methocarbamol, oxycodone.
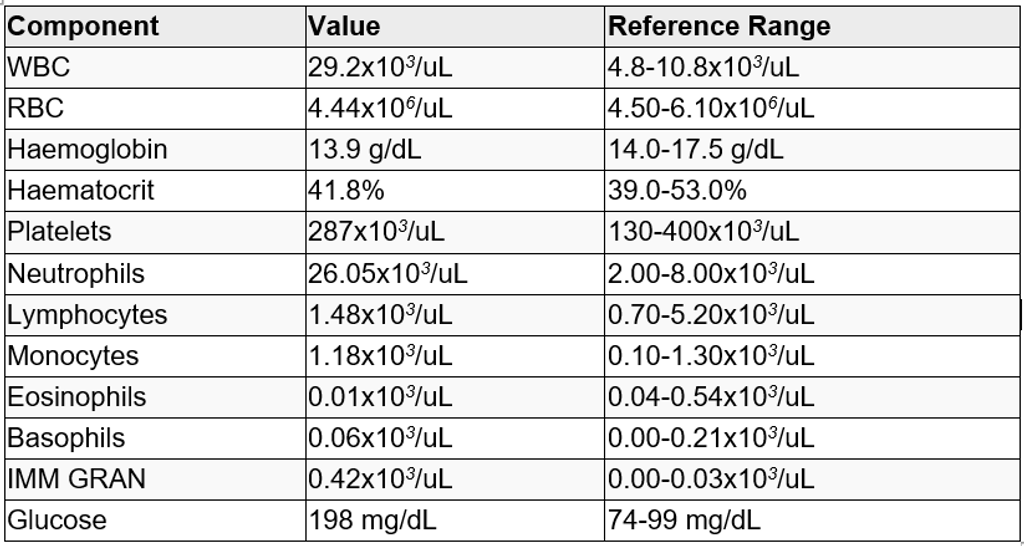
Table 1: CBC with a differential and basic metabolic panel
WBC: white blood cells; RBC: red blood cells; IMM GRAN: immature granulocytes; CBC: complete blood count
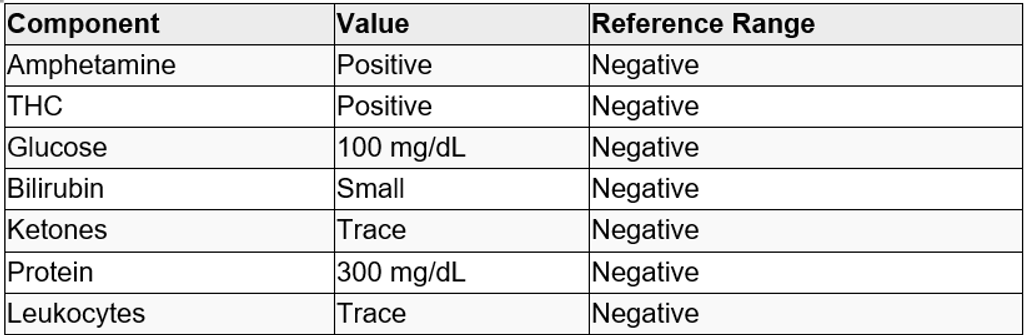
Table 2: Urinalysis and urine toxicology screen
THC: tetrahydrocannabinol
2. Psychiatric Medications:
- Started on lorazepam and olanzapine as needed per the psychiatrist’s recommendation.
Psychiatric Evaluation and Follow-Up
- Initial State: Paranoid, guarded, and insisted on wanting to die.
- Response to Treatment:
- Became calmer and more cooperative after a few days.
- Did not recall the initial meeting with the psychiatrist.
- Consistently monitored on a one-to-one basis.
- Psychiatric Insight:
- Acknowledged extreme paranoia and guardedness under MA influence.
- Recognized lack of a social support system.
- Agreed Treatment Plan:
- Consent to the psychiatric treatment plan before transfer to inpatient psychiatric care.
- Agreed to referrals to community mental health and addiction services.
Discussion
The case of an MA user attempting suicide highlights a critical issue in the broader epidemic of MA use disorder and suicide. This report delves into recent literature on MA use and suicide to identify at-risk populations and develop effective preventive strategies.
Studies conducted in Taiwan using the National Health Insurance Research Data (NHIRD), which covers 99% of the population and is linked to the Taiwan Death Registry (TDR), provide valuable insights. In a cohort of 21,809 MA users, 47.8% were found to have at least one psychiatric disorder, with older women being the most affected demographic [8]. Notably, young women are identified as the group most at risk for suicidal ideation and attempts, and they are also more likely to seek medical help [8,9]. The most prevalent comorbid psychiatric disorders included depression, anxiety, bipolar disorder, and schizophrenia.
Over a 17-year follow-up, the study revealed that MA users with at least one psychiatric disorder had a higher rate of all-cause mortality, with a significant proportion dying from unnatural causes. Shockingly, over half of these unnatural deaths were suicides, and patients with any psychiatric disorder were 2.27 times more likely to die by suicide. These findings underscore the pressing need for targeted prevention efforts, particularly among young women, who are disproportionately affected by the dual burden of MA use disorder and psychiatric comorbidities.
Further analysis of the same database explored all-cause and suicide mortality rates among MA users [10]. It was found that suicide had the highest standardized mortality rate (SMR) among all causes of death in this population, followed by neurological diseases. Interestingly, the study revealed that male MA users had higher cumulative suicide rates compared to females. This might be attributed to the higher prevalence of multiple substance use among men, which had the highest SMR for all-cause mortality. Women, on the other hand, were more likely to have non-substance-related psychiatric disorders. For both genders, suicide attempts were most frequent within the first year after being diagnosed with MA use disorder.
A separate study in Iraq investigated suicide risk factors among crystal MA users [11]. Crystal MA, the purified solid form of the drug, is typically smoked or snorted. Unlike previous studies, this research found no significant difference in suicidal ideation between genders or age groups, possibly due to a limited number of women in the sample. The study highlighted that chronic user (>1 year of use), those experiencing visual hallucinations, episodes of aggression, and abuse of other illicit substances (excluding alcohol) were at a higher risk for suicide.
Interestingly, past trauma showed an inverse relationship with suicide risk, and users with drug-using family members and those using crystal MA in social settings had increased suicide risk.
MA users employ various methods of suicide, which could guide prevention strategies. Although many believe MA-related suicides occur during psychosis, the majority are due to intentional MA overdoses [10]. Other suicide methods more common among MA users compared to the general population include charcoal burning, hanging, drowning, firearms, cutting, and jumping from heights. For female MA users, jumping from high places was the most common method, while males used to hang and charcoal burning more frequently.
In contrast to a Taiwanese study by Lee et al., where about half of the suicides were nonviolent [10], a report from Australia found nearly 70% of MA-related suicides were by hanging [6]. Violent methods such as exsanguination and gunshots were also more frequent among MA users compared to the general population. Toxicology reports did not show significant differences in MA levels by method of suicide, though prescription medications, including sedatives and antidepressants, were commonly found. While violence is often associated with MA use, few studies challenge the link between stimulant drug use and violent behavior [12].
The method of MA use significantly impacts suicide risk. Research from the Vancouver Injection Drug Users Study (VIDUS) revealed that intravenous (IV) MA users are more likely to attempt or complete suicide compared to non-IV users [13]. Younger users and those with shorter injection histories were particularly at risk. Surprisingly, polydrug use did not affect suicide risk among MA users. Hypse’s study found that both infrequent and frequent MA injections were linked to higher suicide rates compared to periods with no MA injection. This highlights the need for further research into the complex relationship between injection frequency and suicide risk [13].
Another important finding is the increased healthcare utilization among MA users before suicide. A case-control study showed that 87% of MA users who committed suicide had accessed health services in the three months leading up to their death [14]. This is a higher rate compared to other substance abuse-related suicides, suggesting a stronger inclination among MA users to seek help. Most visits were to emergency and psychiatric departments, indicating critical points for preventative interventions. Lee et al. also noted that MA users frequently experienced physical and psychiatric comorbidities, such as pneumonia, shortly before their suicides [14]. However, this statistic may be an underestimation, as many MA users avoid healthcare due to legal or social stigma.
Social and medical factors also play a role in MA-related suicide risk. A nested case-control study found that financial independence is a protective factor against suicide [15]. Conversely, visual hallucinations, previous suicide attempts, and depression are significant risk factors. Initiating MA use often stems from stressful life events, psychological trauma, peer pressure, family issues, financial troubles, and marital conflicts [11]. Understanding these risk factors and triggers can enhance screening and treatment strategies for preventing suicide in MA users.
Conclusions
Methamphetamine (MA) use has surged dramatically in recent years, posing a growing health crisis. The drug’s array of medical and psychiatric consequences, particularly its strong link to suicidal thoughts and completed suicides, underscores the urgency of addressing this issue. As MA use increasingly intertwines with various health complications, understanding these patients better is crucial for delivering effective care and implementing preventive strategies.
References
- Espiridion E D, Charron L (July 18, 2024) Methamphetamine Use and Suicide: A Case Report and Brief Review of Literature. Cureus 16(7): e64835. doi:10.7759/cureus.64835
- Executive Summary: World Drug Report 2023. United Nations Office on Drugs and Crime, Vienna, Austria; 2023. https://www.unodc.org/res/WDR-2023/WDR23_Exsum_fin_SP.pdf.
- Han B, Compton WM, Jones CM, Einstein EB, Volkow ND: Methamphetamine use, methamphetamine use disorder, and associated overdose deaths among US adults. JAMA Psychiatry. 2021, 78:1329-42. 10.1001/jamapsychiatry.2021.2588
- Darke S, Kaye S, McKetin R, Duflou J: Major physical and psychological harms of methamphetamine use. Drug Alcohol Rev. 2008, 27:253-62. 10.1080/09595230801923702.
- Marshall BD, Werb D: Health outcomes associated with methamphetamine use among young people: a systematic review. Addiction. 2010, 105:991-1002. 10.1111/j.1360-0443.2010. 02932.x
- Marshall BD, Galea S, Wood E, Kerr T: Injection methamphetamine use is associated with an increased risk of attempted suicide: a prospective cohort study. Drug Alcohol Depend. 2011, 119:134-7. 10.1016/j.drugalcdep.2011.05.012.
- Darke S, Kaye S, Duflou J, Lappin J: Completed suicide among methamphetamine users: a national study. Suicide Life Threat Behav. 2019, 49:328-37. 10.1111/sltb.12442.
- Xing DG, Horan T, Bhuiyan MS, et al.: Social-geographic disparities in suicidal ideations among methamphetamine users in the USA. Psychiatry Res. 2023, 329:115524. 10.1016/j.psychres.2023.115524.
- Fang SC, Hung CC, Huang CY, et al.: Influence of baseline psychiatric disorders on mortality and suicide and their associations with gender and age in patients with methamphetamine use disorder. Int J Ment Health Addiction. 2023, 10.1007/s11469-023-01025-x.
- Bayazit H, Baronia R, Wakefield SM: Methamphetamine intoxication and suicidal ideation/behavior in the emergency department. Curr Med Res Opin. 2024, 40:849-54. 10.1080/03007995.2024.2333429.
- Lee WC, Chang HM, Huang MC, et al.: All-cause and suicide mortality among people with methamphetamine use disorder: a nation-wide cohort study in Taiwan. Addiction. 2021, 116:3127-38. 10.1111/add.15501.
- Al-Imam A, Motyka MA, Hoffmann B, Al-Ka’aby H, Younus M, Al-Hemiary N, Michalak M: Risk factors of suicidal ideation in Iraqi crystal methamphetamine users. Brain Sci. 2023, 13:1279. 10.3390/brainsci13091279.
- Tyner EA, Fremouw WJ: The relation of methamphetamine uses and violence: a critical review. Aggress Violent Behav. 2008, 13:285-97. 10.1016/j.avb.2008.04.005.
- Hypse JD: Suicide rates between methamphetamine users who inject versus non-injectors. J Addiction Res Ther. 2018, 9:359. 10.4172/2155-6105.1000359.
- Lee WC, Chang HM, Huang MC, et al.: Healthcare utilization and psychiatric and physical comorbidities before suicide mortality in patients with methamphetamine use disorder: a nationwide case-control study. Addict Behav. 2022, 126:107192. 10.1016/j.addbeh.2021.107192.
- Kuo CJ, Tsai SY, Liao YT, et al.: Risk and protective factors for suicide among patients with methamphetamine dependence: a nested case-control study. J Clin Psychiatry. 2011, 72:487-93. 10.4088/JCP.09m05360gry
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia.
Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!







