After undergoing a total abdominal hysterectomy (TAH), experiencing intestinal prolapse is rare. This case report highlights the case of a 48-year-old woman who developed intestinal prolapse two weeks after her TAH, resulting in symptoms and a noticeable bulge in the vaginal vault. The problem was effectively addressed through prompt laparotomy. This case emphasizes the significance of maintaining awareness of unusual complications following TAH.
Introduction: The Emergence of Intestinal Prolapse
The term “extra-fascial hysterectomy” is commonly used to refer to total abdominal hysterectomy (TAH). TAH is a surgical procedure employed for various gynecologic conditions, offering a definitive solution for patients seeking relief. Proficiency in TAH is crucial for gynecologists, as the procedure involves the removal of the uterus and carries potential risks such as urinary tract trauma, intestinal tract damage, and bladder injury [1,4].
Adhering to proper release layer protocols and ensuring the genuine removal of the uterus is imperative to prevent surgical complications [1]. The documentation of vaginal cuff dehiscence and evisceration dates back to 1864, with occurrences being rare but significant. Vaginal cuff dehiscence accompanied by evisceration, where organs are expelled through a separated incision, has a frequency ranging from 0.14% to 4.1% [2]. Postoperative complications like vaginal cuff dehiscence and evisceration, especially following pelvic surgery or hysterectomy, require immediate resuscitation and surgical intervention [4].
Vaginal evisceration can manifest at varying intervals post-hysterectomy, emphasizing the need for prompt recognition and management to avoid adverse outcomes [3]. Despite its rarity, understanding occurrences such as intestinal prolapse post-TAH is essential for refining surgical techniques, optimizing postoperative care, and preventing similar complications in future cases.
Elevated abdominal pressure in postmenopausal women and sexual activity in premenopausal patients were identified as common triggering events, with the small bowel being the most frequently eviscerated organ. Patients typically presented with symptoms like a bulging mass, pelvic discomfort, or vaginal bleeding [4]. This case report centers on a 48-year-old woman who underwent an uncomplicated TAH for symptomatic uterine fibroids. Approximately two weeks after discharge, the patient exhibited subtle yet progressive symptoms, ultimately leading to the diagnosis of intestinal prolapse. The intricate clinical course, successful surgical management, and subsequent recovery serve as a focal point for understanding the complexities associated with this uncommon complication.
This report aims to comprehensively explore the patient’s clinical journey, covering symptom onset, diagnostic challenges, surgical intervention, postoperative care, and implications for healthcare practice. By delving into the intricacies of this rare occurrence, the report seeks to contribute to medical understanding regarding uncommon complications post-TAH, stressing the importance of heightened vigilance, meticulous surgical techniques, and tailored postoperative care strategies.
Case Presentation [1]
1. Demographics and Medical History
- Woman’s age: 48 years
- Obstetric history: Three pregnancies, three deliveries
- A recent total abdominal hysterectomy (TAH) was performed 11 weeks before presentation to address uterine fibroids.
2. Urgent Care Visit Triggered by Distressing Symptoms
- Compliance with postoperative instructions
- A distressing episode during a bowel movement, accompanied by vaginal bleeding
- A sensation of something being expelled from the vagina
- Immediate visit to the emergency room prompted by alarming symptoms.
3. Escalating Pelvic Pressure
- Ongoing pelvic pressure over the past few weeks
- Pronounced during bowel movements.
4. Vital Signs and Physical Examination
- Blood pressure: 104/65 mmHg
- Pulse rate: 80 bpm
- Temperature: 37.8 °C
- Respiration rate: 19/minute
- Oxygen saturation: 96% on room air.
5. Physical examination
- No signs of peritoneal irritation (rebound, stiffness, voluntary guarding)
- Moderate to severe suprapubic pain noted.
6. Pelvic Examination Findings
- Distressing discovery of a portion of the small intestine protruding from the upper part of the vaginal area
- Immediate consultation was initiated with the general surgery team due to the severity of the finding.
7. Urgent Workup Recommendation
- Given the potential for severe conditions (e.g., bowel ischemia, early perforation), an urgent and comprehensive workup was advised.
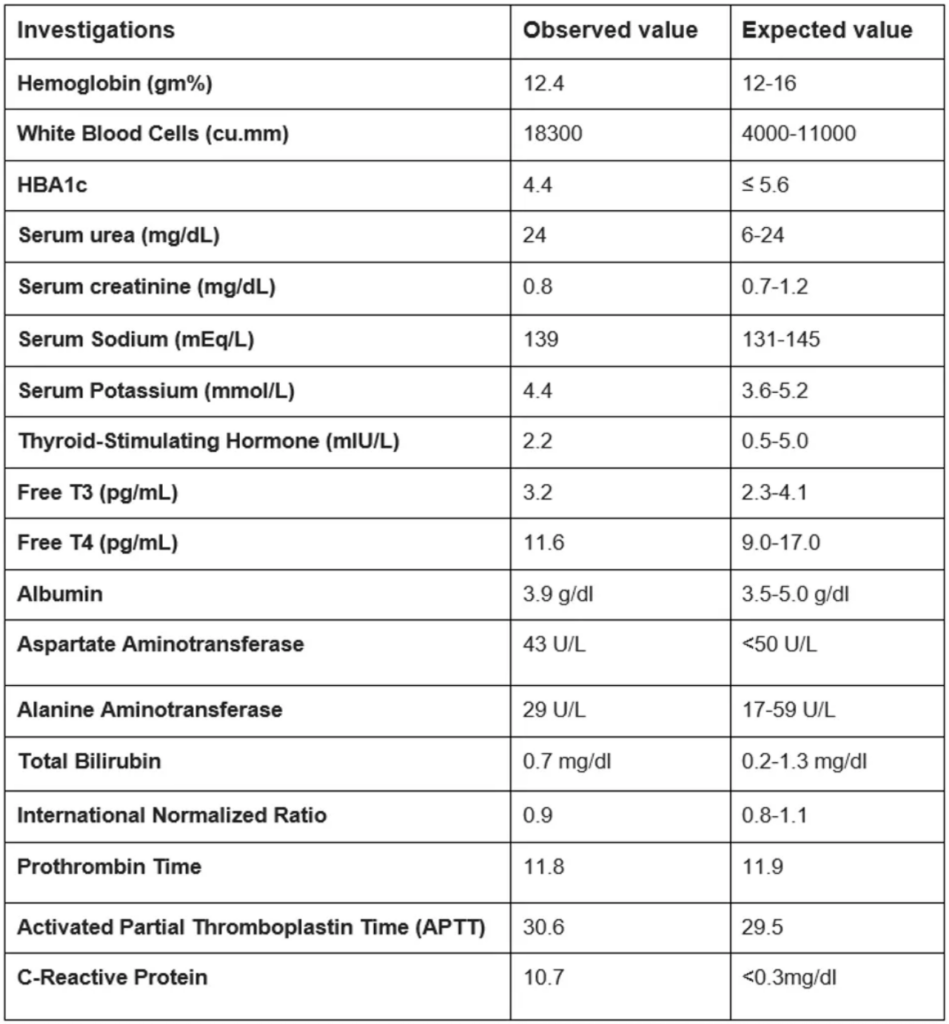
Table 1: List of Diagnostic Tests Conducted on the Patient
8. Laboratory Analysis and Sepsis Indication
- Subsequent laboratory analysis revealed indications of sepsis.
- Prompt initiation of broad-spectrum antibiotics (Total dose: 4.5 grams piperacillin-tazobactam) as per Table 1 in response to the suspected infection.
Surgical Intervention and Postoperative Management [1]
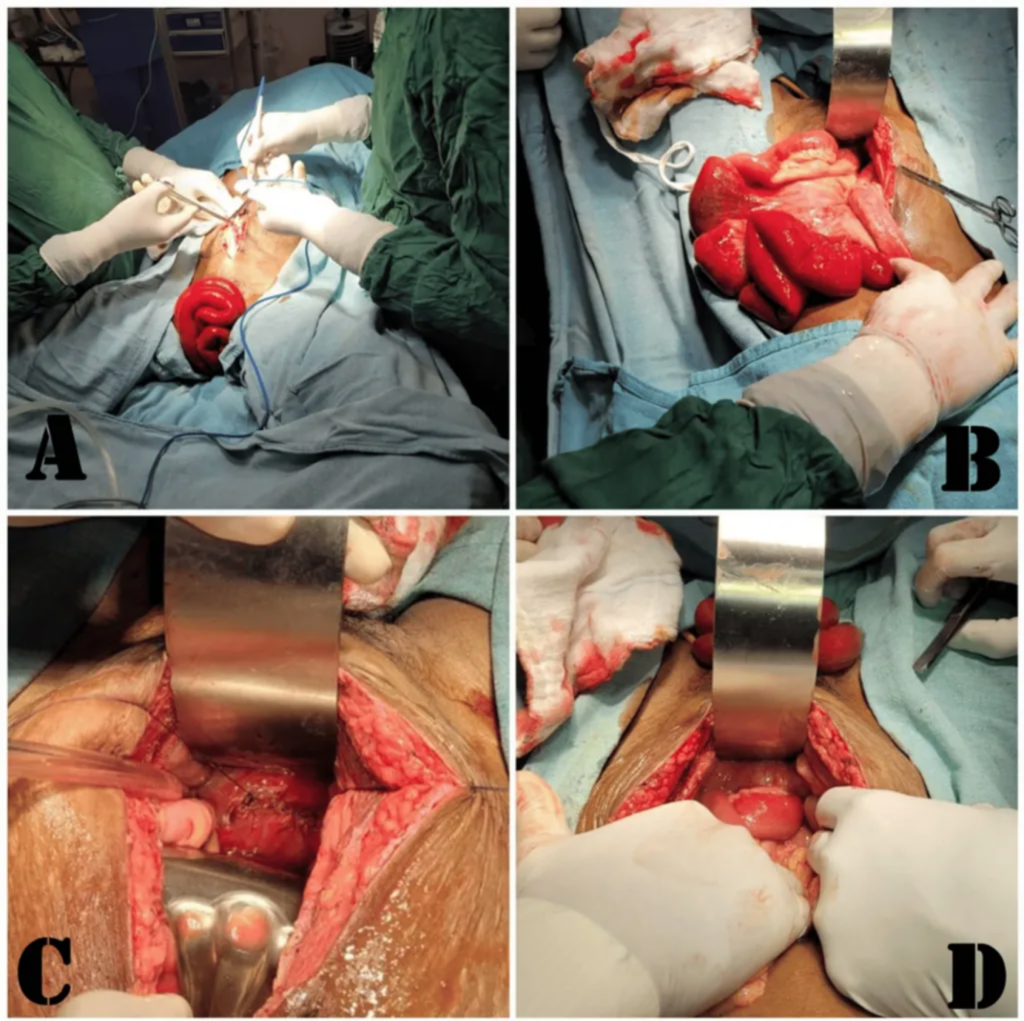
Figure 1: A) Bulging of a small intestinal segment from the vagina, B) careful manual reduction of the eviscerated bowel, C) handling of the vaginal cuff dehiscence, and D) verification of hemostasis before the conclusive closure
1. Swift Arrangement for Urgent Laparotomy
- Urgent surgical intervention conducted via laparotomy under general anesthesia.
2. Intraoperative Examination and Findings
- Careful examination in the operating room revealed complete vaginal cuff dehiscence
- Absence of active infection signs, but identified weaknesses and friability in tissues between the anterior vaginal wall and bladder wall
- Critical intraoperative finding: Segment of small intestine herniating through dehisced vaginal cuff, causing prolapse.
3. Surgical Approach
- Meticulous manual reduction of eviscerated bowel
- Precise management of vaginal cuff dehiscence
- Removal of granulation tissue at vaginal cuff edge
- Meticulous closure using simple interrupted sutures through a vaginal approach
- Careful reduction of prolapsed bowel performed
4. Postoperative Antibiotic Course
- The two-day course of 4.5 grams of piperacillin-tazobactam administered to mitigate infection risk.
5. Postoperative Monitoring and Recovery Focus
- Close monitoring of recovery
- Focus on detecting signs of infection, restoring proper bowel function, and effective pain management.
6. Follow-up Assessments
- Favorable recovery trajectory observed in follow-up assessments
- Resolution of initial distressing symptoms
- Successful management of emergent situations through surgical intervention, as illustrated in Figure 1.
Discussion
The occurrence of intestinal prolapse after a total abdominal hysterectomy (TAH) is an exceedingly rare complication, with limited mentions in the medical literature [5]. This case underscores the importance of clinicians’ vigilance regarding even the most uncommon postoperative complications, especially those impacting the genitourinary system. Despite its rarity, the potential seriousness and the necessity for urgent intervention emphasize the need for a comprehensive understanding of the predisposing factors and effective management strategies associated with this condition [2,5].
Several factors may contribute to intestinal prolapse following total abdominal hysterectomy (TAH). One such factor is the heightened intra-abdominal pressure experienced during the initial postoperative phase. Activities like lifting heavy objects, prolonged straining during bowel movements, or persistent coughing collectively exert excessive pressure on the abdominal cavity, potentially predisposing individuals to intestinal prolapse [6]. Additionally, technical issues or inadequate healing associated with the closure of the vaginal cuff after hysterectomy may make patients susceptible to vaginal cuff dehiscence, facilitating the herniation of intestinal structures.
Recognizing intestinal prolapse as a possible postoperative complication is crucial for timely diagnosis and intervention. Close monitoring during the postoperative recovery and comprehensive patient education on avoiding activities that may increase intra-abdominal pressure serve as vital preventive measures. Moreover, meticulous attention to surgical techniques during vaginal cuff closure is imperative to minimize the risk of dehiscence and subsequent complications [7, 8].
In cases where intestinal prolapse occurs, urgent surgical intervention becomes imperative. Timely reduction of the prolapsed bowel, followed by meticulous repair of the vaginal cuff, is essential for achieving a favorable postoperative outcome. Subsequent postoperative care involves vigilant monitoring for signs of infection, restoration of bowel function, and effective pain management to facilitate patient recovery and alleviate discomfort [4,6].
While this case highlights successful management, further research is necessary to elucidate preventive strategies and refine surgical techniques. Prospective studies evaluating optimal methods for vaginal cuff closure, strategies for mitigating intra-abdominal pressure post-hysterectomy, and long-term outcomes in similar cases would undoubtedly provide invaluable insights into minimizing the incidence of such rare complications [9]. In summary, ongoing research initiatives and clinical diligence are indispensable in addressing and managing intestinal prolapse following TAH, ensuring optimal patient outcomes and quality of care.
Conclusion
This case highlights intestinal prolapse following total abdominal hysterectomy and underscores the importance of vigilant postoperative monitoring and risk awareness. The patient’s journey, successful surgical intervention, and recovery provide valuable insights into this uncommon issue. Timely recognition and intervention proved pivotal for a positive outcome, emphasizing the necessity for prompt action in addressing such complications. This case underscores the need for further research to refine surgical techniques and postoperative care to prevent similar incidents after hysterectomy. Heightened awareness and ongoing studies are essential for advancing patient care and outcomes in gynecologic surgeries, particularly in addressing rare complications like intestinal prolapse.
References
- Singh Thakur A, Tayade S, Gupta V K, et al. (February 09, 2024) An Unforeseen Complication: Intestinal Prolapse After Total Abdominal Hysterectomy. Cureus 16(2): e53922. doi:10.7759/cureus.53922
- Hiramatsu Y: Basic standard procedure of abdominal hysterectomy: part 1. Surg J (NY). 2019, 5: S2-S10. 10.1055/s-0039-1678575
- Chen HY, Sheu BC, Chang WC: Prolapsed epiploic of bowel after robotic hysterectomy: a case report. Ann Med Surg (Lond). 2020, 60:146-8. 10.1016/j.amsu.2020.10.055
- Thomopoulos T, Zufferey G: Totally laparoscopic treatment of vaginal cuff dehiscence: a case report and systematic literature review. Int J Surg Case Rep. 2016, 25:79-82. 10.1016/j.ijscr.2016.06.004
- Ramirez PT, Klemer DP: Vaginal evisceration after hysterectomy: a literature review. Obstet Gynecol Surv. 2002, 57:462-7. 10.1097/00006254-200207000-00023
- Lawson L, Patterson L, Carter K: Transvaginal evisceration progressing to peritonitis in the emergency department: a case report. Int J Emerg Med. 2011, 4:66. 10.1186/1865-1380-4-66
- Apicella M, Mayrink M, Rajadhyaksha CD, Farcy DA: A case of transvaginal small bowel evisceration following hysterectomy with discussion of emergency department diagnosis and management. Case Rep Emerg Med. 2022, 2022:1334302. 10.1155/2022/1334302
- Nasr AO, Tormey S, Aziz MA, Lane B: Vaginal herniation: A case report and review of the literature. Am J Obstet Gynecol. 2005, 193:95-7. 10.1016/j.ajog.2004.12.022
- Cruickshank L, Amin A, DeSilva A: Small bowel evisceration: a late complication following vaginal hysterectomy. J Obstet Gynaecol. 2018, 38:733. 10.1080/01443615.2018.1444397
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!







