Hot Tub Lung (HTL) is a rare pulmonary condition caused by inhaling aerosolized non-tuberculous mycobacteria (NTM) typically found in hot water steam. This disease can strike both healthy and immunocompromised individuals. Diagnosing HTL requires high clinical suspicion, high-resolution computed tomography (HRCT), and microbiological evidence. In an unprecedented case, we report the only known instance of HTL linked to an indoor swimming pool, affecting five family members, including one non-resident.
Introduction: Hot Tub Lung and Environmental Mycobacteria
This case highlights an unusual hot tub lung (HTL) outbreak in five family members, all linked to aerosolized non-tuberculous mycobacteria (NTM) from their indoor swimming pool.
Case Presentation
- Patient Profile: 17-year-old male, admitted ten days post-ankle reconstruction, less than seven days since discharge.
- Symptoms: Cough, low-grade fevers, progressively worsening dyspnea.
- Initial Presentation: Tachypnea with exercise-induced hypoxemia (SpO2: 82%) during short walks.
- Noteworthy Exclusions: No viral symptoms, systemic symptoms (rashes, joint pain, hematuria), prior medical or respiratory history, recent travel, or sick contacts.
- Family Health:
- Younger brother (14) recently had a cough with dyspnea.
- Mother experienced a persistent cough over the last three months.
- Physical Examination: Extensive bilateral crackles on chest auscultation, no signs of heart failure.
- Treatment: Supplemental oxygen via nasal cannula at 3 L/min is required to maintain oxygen saturation above 90%.
Key Investigations and Findings
- Blood Work Results:
- Mild neutrophilia: 8.6 × 10⁹/L
- Eosinophilia: 1.17 × 10⁹/L
- Mildly elevated C-reactive protein (CRP): 10 mg/L
- Infection Search: Extensive and all negative
- Blood cultures
- Respiratory virus PCR
- Urinary Legionella and Streptococcus pneumoniae antigens
- Mycoplasma IgM
- Chlamydia psittaci and Chlamydia pneumoniae IgG
- Aspergillus and avian precipitin studies
- Autoimmune Screen: Negative
- Pulmonary Function Tests:
- Restrictive pattern impairment
- FEV1: 2.52 L (64% predicted)
- FVC: 3.42 L (72% predicted)
- DLCO: 19.54 mL/min/mmHg (67% predicted)
- CT Chest scan:
- Bilateral, symmetrical, diffuse patchy ground-glass opacities
- Associated small-volume adenopathy
- No micronodularity was observed in (Fig.1)
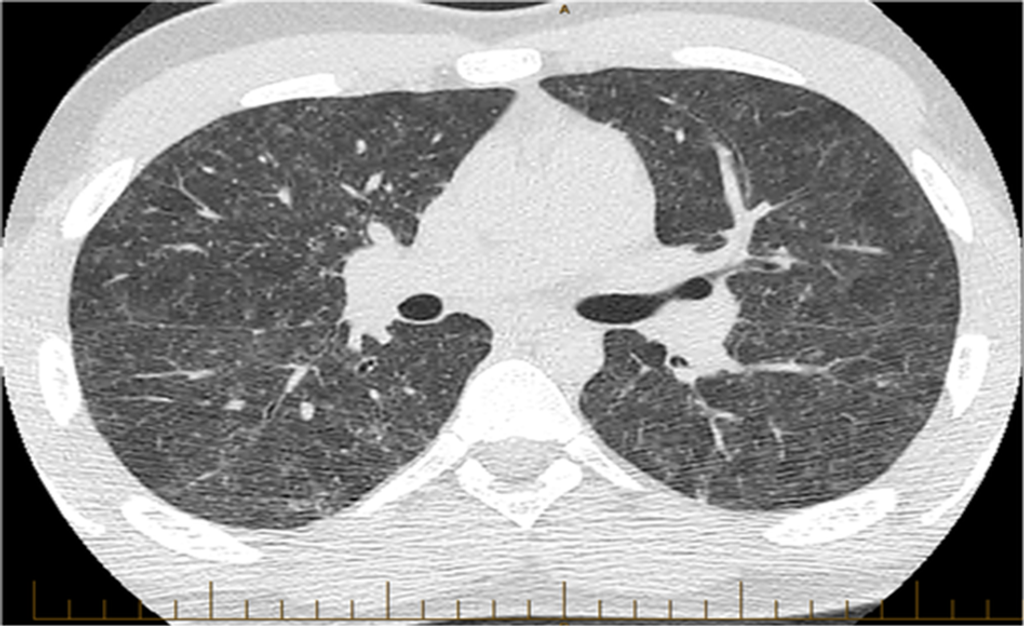
Figure 1: Computed tomography (CT) scan of the patient at diagnosis demonstrating bilateral, symmetrical, diffuse patchy ground-glass opacities with associated small volume adenopathy, consistent with hypersensitivity pneumonitis (HP)-associated non-tuberculous mycobacteria (NTM) infection.
- Environmental Investigation:
- The family’s indoor pool recently switched from chlorine-based sanitation to a non-chlorine (Perox and hybrid ozone) system.
- The occupational hygienist found:
- Mould (Scedosporium spp.) due to excess humidity in the house.
- Pet cockatiel in the kitchen area.
- Additional mould (Cladosporium spp.) was identified through microscopic analysis.
- No other water sources are suspected of potential exposure.
- Preliminary Diagnosis:
- Hypersensitivity pneumonitis (HP) is suspected based on environmental antigens and the patient’s clinical course.
- Negative tests for HP antigens (Micropolyspora faeni, terrestrial actinomycetes, pigeon serum IgG, Penicillium, Cladosporium, Candida albicans, Alternaria, and Setomelanomma).
- No elevation in specific IgE and IgG Aspergillus antibodies.
- Bronchoalveolar Lavage (BAL) Results:
- Lymphocytosis (36%) without eosinophilia (0%).
- Standard culture: no pathogens grown.
- Corticosteroids were withheld due to daily improvement with supportive care.
- Water Testing:
- Environmental testing of pool water by Mycobacterial Reference Laboratory at Royal Brisbane and Women’s Hospital.
- Main water sources (kitchen, bathrooms, showers) were also tested.
- Microbial Findings:
- Mycobacterium intracellulare was cultured from the patient’s BAL sample and indoor pool water.
- Mycobacterium avium and Mycobacterium marinum are found in pool water, not house water.
- Ensuite shower water grew Mycobacterium lentiflavum.
- No other water sources tested positive.
- Outcomes:
- Diagnosis of Hot Tub Lung (HTL) supported by the presence of Mycobacterium intracellulare in both patient and pool water samples.
- Property and Pool Cleaning:
- Commercial cleaning and disinfection are conducted per local health authority guidelines.
- Procedures included:
- Residual chlorination
- Super chlorination
- Chemical cleaning
- Pasteurization
- Treatment and Follow-up:
- Antimicrobial therapy is not required.
- The main treatment involved close follow-up and removal of environmental antigens.
- Patient Outcomes:
- Lung function tests improved to stable, low normal values:
- FEV1: 3.98 L (88% predicted)
- FVC: 4.96 L (93% predicted)
- DLCO: 27.16 (74% predicted)
- A high-resolution CT (HRCT) scan over two years showed normal results (Fig.2).
- Lung function tests improved to stable, low normal values:
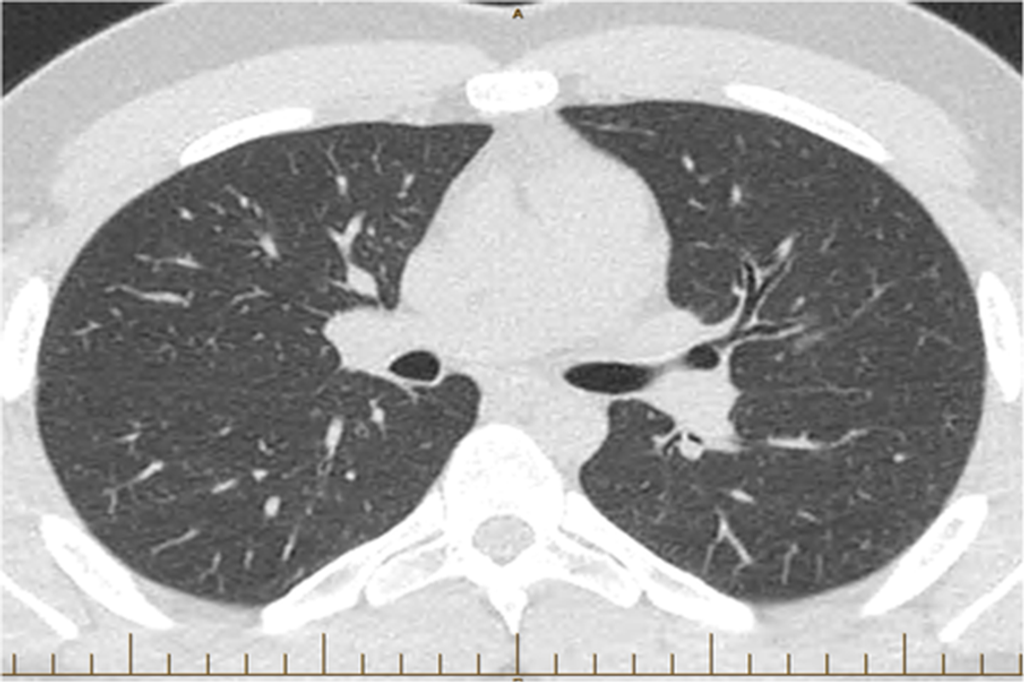
Figure 2: High-resolution computed tomography (HRCT) scan of the patient at two years follow-up demonstrating resolution of the prior changes.
15. Family Health Observations:
- The patient’s parents, younger brother, and grandmother developed persistent coughs and varying degrees of dyspnea.
- Gas transfer values: 50–60% predicted for all affected family members.
- Radiological findings consistent with NTM disease:
- Subpleural nodular changes in younger brother and grandmother.
16. Mother’s additional symptoms:
- Sweats
- Class I dyspnea
- BAL and biopsies:
- No Mycobacterium isolated
- Interstitial granulomatous inflammation with punctate necrosis, consistent with mycobacterial infection
17. Treatment and Follow-up:
- The family was treated conservatively due to normal immune function.
- Grandmother frequently visited but did not live at the residence.
- Two-year follow-up: no residual respiratory symptoms in family members.
- Pulmonary function tests showed a persistent mild reduction in DLCO.
18. Patient’s Symptom Progression:
- Symptoms are believed to have been present for months.
- Acute deterioration post-operatively, coinciding with extended time in a media room adjacent to the pool.
Discussion & Conclusions
Non-tuberculous mycobacteria (NTM) hide in soil, natural water bodies, and municipal water supplies. Diagnosing an NTM infection can be tricky since it can mimic other clinical conditions. While it’s rare for these bugs to spread through the air, particularly in healthy individuals, they can become airborne and inhaled from sources like hot tub steam, leading to a condition called “hot tub lung.”
Spotting NTM infections requires a keen eye, combining clinical suspicion with radiological and microbiological evidence. Treatment varies, ranging from conservative approaches to corticosteroids and long-term antibiotics, depending on the individual’s immune status, the specific mycobacterium, radiological findings, and disease severity. Although permanent lung changes can occur, healthy individuals typically have good long-term outcomes.
This case underscores the importance of considering environmental factors when investigating clusters of pulmonary disease.
References
- Griffith DE, Aksamit T, Brown-Elliott BA, et al. 2007. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respir. Crit. Care Med. 175(4): 367–416.
- Porvaznik I, Solovič I, and Mokrý J. 2016. Non-tuberculous mycobacteria: classification, diagnostics, and therapy. Pp. 19–25 in M. Pokorski, ed. Respiratory Treatment and Prevention. Cham, Switzerland, Springer International Publishing. Available at: http://link.springer.com/10.1007/5584_2016_45 (accessed 8 January 2020).
- Haworth CS, Banks J, Capstick T, et al. 2017. British Thoracic Society guidelines for the management of non-tuberculous mycobacterial pulmonary disease (NTM-PD). Thorax 72(Suppl. 2): ii1–ii64.
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!







