Sickle cell disease (SCD) is a complex group of genetic haemoglobin disorders with far-reaching effects on multiple body systems. This report focuses on practical strategies for managing SCD in children and teens, offering essential guidance for paediatric primary care providers. While it doesn’t dive into every complication, it highlights key areas that require close attention. The take-home message? Fast, appropriate treatment is crucial when acute illness strikes, as life-threatening complications can escalate quickly.
Comprehensive, specialised care—delivered by a dedicated team—has been proven to reduce childhood morbidity and mortality. This collaborative care approach involves much more than routine checkups; it includes patient and family education, regular evaluations, health maintenance services, psychosocial support, genetic counselling, and nursing care. Ideally, paediatricians or primary care providers work with SCD specialists, including haematologists, nurse specialists, social workers, and educational liaisons, to ensure the best possible outcomes.
Overview of Sickle Cell Disease (SCD)
SCD is a group of chronic, complex disorders that bring unpredictable challenges—from life-threatening complications to long-term organ damage. While expert care significantly reduces these risks and improves life expectancy, many children and teens with SCD rely on paediatricians for their primary medical support. This report offers a practical guide to paediatric primary care providers, outlining the key components of comprehensive care for young patients with SCD. Though based on expert consensus rather than a systematic review, it delivers essential strategies to anticipate and manage complications, ensuring healthcare providers and families feel confident in the care process.
SCD originated in West Africa over 50,000 years ago, offering some protection against cerebral malaria. It spread across the globe through migration and the transatlantic slave trade, and today, it affects people from diverse regions, though it has long been viewed as a disorder primarily impacting communities of colour. Unfortunately, access to quality care has been hindered by socioeconomic inequality, underfunded research, and systemic racism. The effects of racism—whether institutional or personal—continue to influence the care provided to those with SCD negatively.
While long-term societal changes are necessary to overcome these issues, healthcare providers can begin addressing them now. The first step is eliminating “sickler” and encouraging mindful, bias-aware practices. By fostering a compassionate, inclusive environment and actively addressing SCD patients’ unique challenges, medical providers can help build the trust essential to overcoming these systemic barriers.
Despite advances in care, the median life expectancy for individuals with sickle cell anaemia (HbSS) remains in the fifth decade, about 20 years less than their peers without SCD. This report aims to promote equity in care and equip healthcare providers with the knowledge to improve outcomes for all patients with SCD.
1. Newborn Screening and Initial Diagnosis
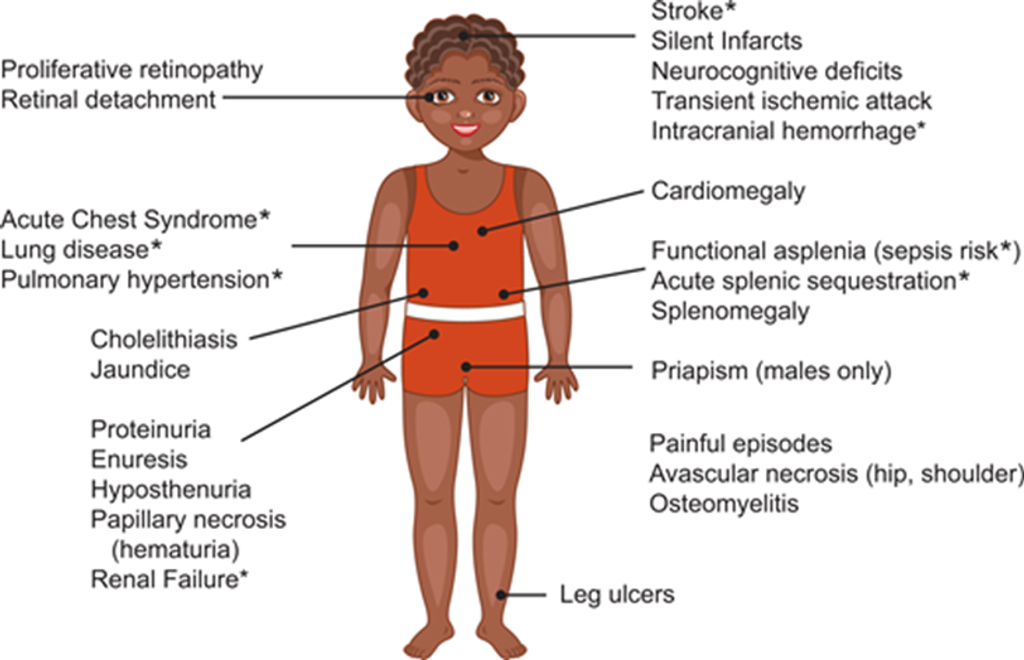
Figure 1: Complications of SCD. Additional complications: Anaemia, delayed growth, and sexual maturation. *Potential cause of mortality. (Yates et al. 2024)
Newborn Screening (NBS)
- SCD diagnosis at birth via NBS.
- Age: 0–3 months.
- Pediatric consultation and referral to an SCD specialist (pediatric hematologist).
Action Plan:
- Immediate referral to pediatric hematologist by 3 months of age.
- Education for family: Explain genetic implications, inheritance patterns, and future pregnancy risks.
Key Points:
- Comprehensive care should begin early.
- Parents should understand the diagnosis, prognosis, and genetic risk for future children.
2. Health Maintenance and Regular Check-Ups
Visit Frequency:
- Infants (0-12 months): SCD-specific visits every 2-4 months.
- Children (1-21 years): SCD-specific visits every 6-12 months.
- Assessment: Growth, neurodevelopment, physical exams, vaccinations, and blood work.
Action Plan:
- Monitor hemoglobin levels, reticulocyte counts, and spleen palpation.
- Administer routine vaccinations, including additional vaccines for children with functional asplenia (e.g., pneumococcal and meningococcal vaccines).
Key Points:
- Routine CBC and reticulocyte counts are essential for disease monitoring.
- Family education should be continuously reinforced.
3. Acute Illness Management
Acute Fever (≥38°C):
- Fever can be life-threatening due to the risk of infection.
- Immediate actions: CBC, blood cultures, reticulocyte count, and antibiotics (ceftriaxone).
- Admit to hospital if necessary.
Action Plan:
- Urgent evaluation of febrile patients with SCD.
- Initiate antibiotics promptly and closely monitor for sepsis.
Key Points:
- Splenic dysfunction increases the risk of infections.
- Comprehensive baseline information should be readily available for acute management.
4. Pain Crisis Management
Vaso-occlusive Pain Episodes:
- Episodes managed at home with oral fluids, NSAIDs, and warmth.
- Severe pain: Hospitalisation, intravenous fluids, and parenteral opioids.
- Monitor for complications like Acute Chest Syndrome.
Action Plan:
- Ensure rapid assessment and aggressive pain management.
- Use opioids for severe pain, avoid delays in care due to stigma surrounding pain relief.
Key Points:
- Severe pain requires aggressive management, often using patient-controlled analgesia.
- Pain crises can precede life-threatening complications.
5. Chronic Disease Management: Hydroxyurea
Hydroxyurea Therapy:
- Offered from 9 months of age for HbSS or Sb0-thalassemia.
- Reduces vaso-occlusive episodes, Acute Chest Syndrome, and improves overall outcomes.
- Regular CBC and reticulocyte monitoring for myelosuppression.
Action Plan:
- Educate families about the benefits of early hydroxyurea initiation.
- Regularly monitor blood counts and adjust dosages accordingly.
Key Points:
- Hydroxyurea is standard therapy and should be part of routine management.
- Continuous reassessment of adherence and side effects is crucial.
6. Transcranial Doppler Screening for Stroke
Stroke Risk Screening:
- Annual Transcranial Doppler (TCD) from 2–16 years of age for children with HbSS and Sb0-thalassemia.
- Elevated TCD velocity indicates high stroke risk.
Action Plan:
- Perform TCD annually.
- Initiate chronic transfusion therapy for stroke prevention if indicated by TCD results.
Key Points:
- TCD screening is vital for primary stroke prevention.
- Transfusion protocols should be established for children with elevated risk.
Health Supervision from Birth to Early Adulthood
Advances in care have enabled most children with SCD to reach adulthood and transition to adult care, allowing a new focus on enhancing quality of life. Providing optimal care is a team effort, requiring collaboration between the paediatric primary care provider and the haematology specialist. Throughout all stages of life, psychosocial support plays a crucial role, with increasing access to online resources. This guideline outlines the recommended care for children with SCD from birth through the transition to adult care, highlighting key aspects of health maintenance and patient/family education.
Reference
Yates AM, Aygun B, Nuss R, Rogers ZR; Section on Hematology/Oncology; AMERICAN SOCIETY OF PEDIATRIC HEMATOLOGY/ONCOLOGY. Health Supervision for Children and Adolescents with Sickle Cell Disease: Clinical Report. Pediatrics. 2024;154(2): e2024066842. doi:10.1542/peds.2024-066842
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia.
Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!







