Idiopathic hypersomnia (IH) is a central disorder characterized by excessive daytime sleepiness, where individuals experience an overwhelming urge to sleep and wake up feeling non-refreshed despite adequate sleep duration. Debate has surrounded this condition’s classification and diagnostic criteria in the past. Presently, subtypes are categorized based on total sleep time:
→ Idiopathic Hypersomnia with long sleep time
→ Idiopathic Hypersomnia without long sleep time
While IH diagnosis relies on exclusion, electrophysiological tests such as polysomnography and mean sleep latency test are pivotal in confirming it. This underscores the importance of an interdisciplinary approach involving various healthcare professionals in the evaluation and management of patients with idiopathic hypersomnia.
Objectives
- Describe signs and symptoms of idiopathic hypersomnia.
- Outline differential diagnoses of hypersomnolence.
- Summarize the diagnostic criteria.
- Review treatment options for idiopathic hypersomnia.
Introduction
Idiopathic hypersomnia (IH), first identified by Bedrich Roth in Prague in 1956, stands as a rare chronic sleep disorder [1]. It is characterized by persistent excessive daytime sleepiness, an irresistible urge to nap extensively, and frequent difficulty awakening despite having slept for average or prolonged periods at night for a minimum of three months [2].
Considered a neurological disorder, IH is classified as a central disorder of hypersomnolence alongside narcolepsy (both type 1 and type 2) and Kleine-Levin syndrome [2]. Despite its recognition, the precise pathophysiology of IH remains poorly understood, posing challenges for clinicians in diagnosis and management.
This article explores the etiology, epidemiology, clinical manifestations, and treatment approaches for IH in adults.
Etiology
The exact cause of IH remains unclear, but various factors are believed to contribute to its onset. These include sudden changes in sleep-wake patterns, excessive physical exertion, general anesthesia administration, viral infections, and mild head injuries [3]. Recently, emerging evidence suggests a potential genetic predisposition to IH, particularly involving variants affecting orexin signalings, such as those occurring at the cleavage site of pre-pro-orexin and the homozygous PER2 variant [4,5].
Moreover, research indicates that microRNA (miRNA) dysregulation may also be implicated in developing central hypersomnia, including IH [6]. Additionally, recent studies have suggested a possible connection between IH and abnormal immune responses triggered by interactions between vaccine antigens and neural cell antigens reminiscent of those observed in narcolepsy [7].
Epidemiology
While central hypersomnia is viewed as a spectrum, the prevalence of its subtypes varies. Idiopathic hypersomnia (IH) exhibits the lowest occurrence compared to narcolepsy type 1 and type 2, constituting approximately 82%, 13%, and 5%, respectively [8]. Usually, IH is categorized as a neurological disorder falling under the classification of central disorders of hypersomnolence. Other disorders within this classification include narcolepsy (both type 1 and type 2) and Kleine-Levin syndrome, which predominantly affects adolescents and young individuals, with the average age of symptom onset at 17 years and diagnosis at 30 years.
Around one-third of IH cases have a familial predisposition, with family members often experiencing IH or other central hypersomnolence disorders like narcolepsy [1]. Over the past decade, there has been a notable 32% increase in the prevalence of IH, affecting both men and women equally, with rates rising from 7.8 to 10.3 cases per 100,000 individuals [9].
Pathophysiology
Neurochemical investigations yield inconclusive results. The primary pathophysiological characteristic of central hypersomnia appears to be a dysfunction in the central nervous system’s arousal mechanism rather than overactivity in sleep centers [10].
In narcolepsy with Cataplexy (narcolepsy type 1), a significant pathology involves the impairment of orexin neurotransmission. Orexin, a neuropeptide predominantly synthesized by neurons in the lateral hypothalamus, is believed to undergo disruption, possibly due to an autoimmune reaction [11]. However, the underlying pathophysiology of other central hypersomnia’s, like idiopathic hypersomnia, remains elusive.
History and Physical
The usual presentation includes persistent and severe daytime sleepiness in teenagers or young adults, often accompanied by episodes of “sleep drunkenness,” making it hard to wake up with temporary confusion. Symptoms develop gradually over weeks to months, which makes it difficult to identify specific triggers.
Patients often mention long daytime naps (more than one hour) that don’t make them feel refreshed, although sudden sleep attacks are rare. In the second edition of the International Classification of Sleep Disorders (ICSD), two clinical types of idiopathic hypersomnia (IH) were recognized: IH with long sleep time (IHwLST, more than 10 hours) and IH without long sleep time (IHwoLST). Those who sleep longer (over 10 to 11 hours) tend to be younger when symptoms start, have lower weight, and better sleep quality.
In the IHwLST group, the onset of the disease is generally reported to occur at a younger age, and individuals tend to have longer Mean Sleep Latency Test (MSLT) latency, with naps that do not provide refreshment [14].
While excessive daytime sleepiness is the primary characteristic of IH, its symptoms extend beyond this and often persist despite treatment. Specifically, those with IHwLST may also experience severe sleep inertia, fatigue, and a tendency toward evening chronotype. Additionally, a study involving five hundred sixty-three participants with idiopathic hypersomnia found that brain fog and sleep drunkenness were more prevalent in individuals with IH characterized by longer sleep durations [12]. Other symptoms, such as automatic behaviors, sleep paralysis, and hypnagogic hallucinations, are common but lack specificity.
In comparison to narcolepsy, individuals with IH are more likely to have prolonged and non-refreshing daytime naps and may have a family history of sleepiness. Polysomnography typically reveals increased slow-wave sleep, and individuals often exhibit longer sleep latency on the multiple sleep latency test [15].
Evaluation
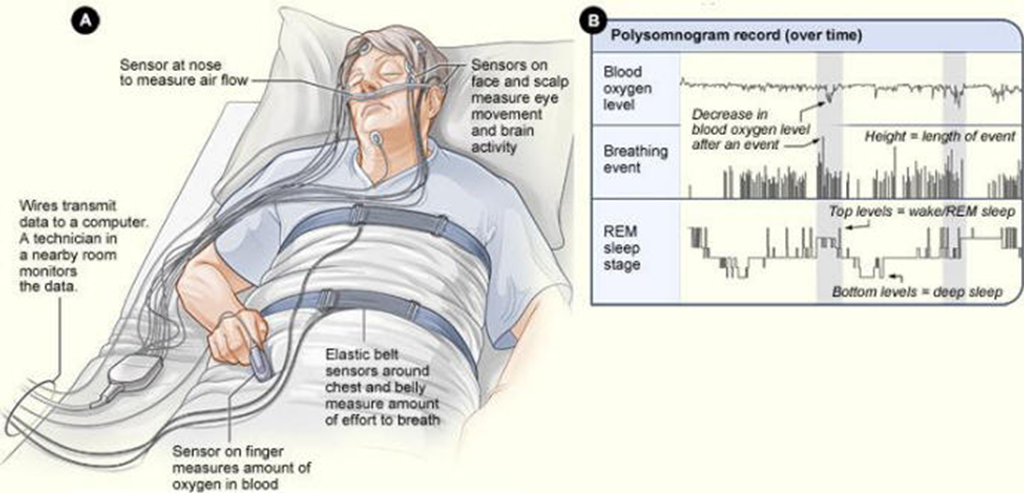
Diagnosing IH involves excluding other potential causes of hypersomnia, as history alone is insufficient for its determination [16]. Hence, objective tests like polysomnography (PSG) and multiple sleep latency tests (MSLT) are important. These tests measure mean sleep latency and the occurrence of sleep-onset REM periods (SOREMs), complemented by wrist actigraphy and sleep logs. They differentiate IH from similar disorders like depression, insufficient sleep, sedative medication use, and sleep-related breathing issues.
A minimum total sleep time of 660 minutes is typically required, especially when the mean sleep latency on the MSLT exceeds 8 minutes. However, the MSLT is not highly sensitive for diagnosing IH [1]. PSG commonly reveals short sleep latency, increased total sleep time (TST), spindles, and improved sleep efficiency. Furthermore, it aids in excluding sleep-disordered breathing (SDB) and identifying SOREMs in narcolepsy.
A valid MSLT must be conducted on the day following a nocturnal PSG session during which the subject has slept for at least 6 hours. In cases of IH, the MSLT typically comprises five daytime nap opportunities, with a mean sleep latency of fewer than 8 minutes accompanied by either sleep-onset REM Periods (SOREMPs) or fewer than two.
Actigraphy can provide valuable assistance by conducting multiple-day recordings within a home environment, thereby corroborating the history obtained through sleep logs, ideally spanning at least seven days with unrestricted sleep.
Cerebrospinal fluid (CSF) hypocretin testing is generally unnecessary and is primarily utilized to confirm the diagnosis of narcolepsy rather than IH. If suspicion regarding an accurate diagnosis persists, repeating the MSLT may be necessary.
As outlined in the third edition of the International Classification of Sleep Disorders (ICSD), the diagnostic criteria include:
- Daily occurrences of an irresistible urge to sleep.
- No Cataplexy.
- MSLT shows a mean sleep latency of less than 8 minutes or total sleep time (TST) exceeding 660 minutes on 24-hour polysomnography (PSG) or actigraphy combined with a sleep log.
- No evidence of insufficient sleep based on the sleep diary.
- MSLT results in symptoms of hypersomnolence that cannot be attributed to another cause [2].
Treatment & Management
Non-pharmacological interventions, such as extending sleep duration, implementing scheduled naps, and engaging in behavioral therapy, generally exhibit limited effectiveness.
Pharmacological treatment, on the other hand, has proven efficacy and includes medications aimed at enhancing alertness:
Modafinil: According to the most recent clinical guidelines from the American Academy of Sleep Medicine, modafinil is recognized as the primary therapeutic choice for idiopathic hypersomnia [17]. Its effectiveness in treating IH mirrors that observed in cases of narcolepsy and is considered very safe, even for individuals with normal sleep durations [Level I evidence] [18,19].
Commonly reported adverse effects include headaches and gastrointestinal disturbances. Modafinil has been shown to significantly reduce self-reported daytime sleepiness on the Epworth Sleepiness Scale by an average of 5.08 points more than placebo (95% confidence interval [CI] 3.01 to 7.16). Additionally, modafinil improves the ability to maintain wakefulness on the Maintenance of Wakefulness Test by an average of 4.74 minutes more than placebo (95% CI 2.46 to 7.01).
Other Medications for Idiopathic Hypersomnia:
- Oxybate was assessed in a phase 3 multicenter study conducted across six European Union countries and the USA. This study employed a placebo-controlled, double-masked, randomized withdrawal design. The administration of a low-dose oral solution of oxybate once or twice nightly, with dose adjustments ranging from 2.5 to 9.0 g per night, proved effective in reducing sleepiness. The Epworth Sleepiness Scale (ESS) scores decreased significantly from a mean of 15.7 (SD 3.8) at baseline to 6.1 (SD 4.0) [Level I evidence] [20].
- Reported adverse events included nausea (22%), headache (18%), dizziness (12%), anxiety (11%), and vomiting (11%).
- Mixed oxybate salts received FDA approval in 2021 [21].
- It is recommended to initiate oxybate treatment at a low dose of less than 3 g and titrate slowly, increasing by no more than 1.5 g per night per week.
- Amphetamines: Includes central nervous system stimulants such as methylphenidate, are utilized in the management of certain sleep disorders [Level V evidence] [22].
- Other stimulants: Pitolisant, a selective histamine H3 receptor antagonist, has been approved for the treatment of narcolepsy with or without Cataplexy. It may also potentially address specific cases of idiopathic hypersomnia [Level V evidence] [23].
- Clarithromycin: It was investigated in a trial involving 20 participants with various sleepiness disorders, including 10 individuals diagnosed with idiopathic hypersomnia, with or without prolonged sleep time. The trial compared clarithromycin to a placebo [24]. Notably, no significant differences were observed between clarithromycin and placebo across measures such as the Epworth Sleepiness Scale, psychomotor vigilance testing, sleep inertia, subjective ratings, or adverse effects [Level 5 evidence].
- Flumazenil: It functions as a GABA-A receptor antagonist when administered sublingually or transdermally. A retrospective chart review study provided evidence of its effectiveness in reducing sleepiness in refractory cases of hypersomnia [Level V evidence] [24].
As per the latest clinical practice guidelines from the American Academy of Sleep Medicine (AASM) for managing central disorders of hypersomnolence, modafinil is strongly recommended as the primary treatment choice for idiopathic hypersomnia in adults. Alternative options for treating idiopathic hypersomnia in adults, including clarithromycin, methylphenidate, pitolisant, and sodium oxybate, received a conditional recommendation [17].
Differential Diagnosis
- Insufficient Sleep: Extending sleep duration before testing is a helpful strategy.
- Drugs/Substance Use.
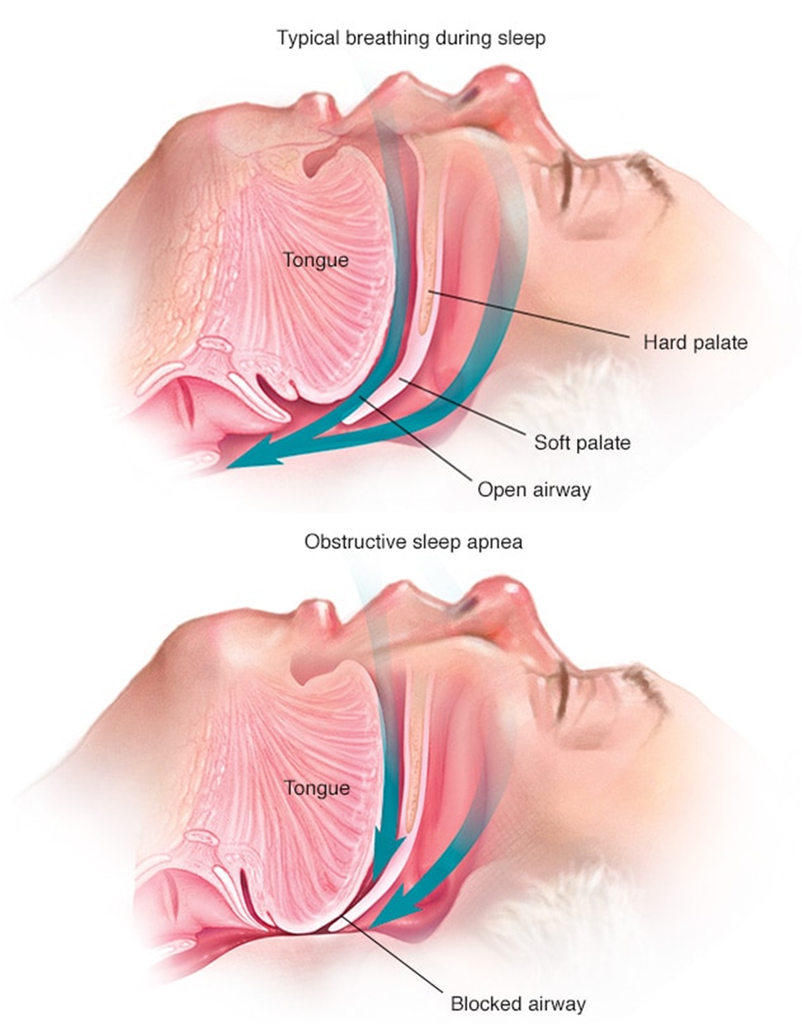
- Sleep-Related Breathing Disorder: Polysomnography is necessary to confirm this diagnosis. Idiopathic hypersomnia should only be considered after adequate treatment and adherence are ensured.
- Narcolepsy Type 2 (Without Cataplexy): Sleep Onset REM Periods (SOREMPs) may not be present during the Multiple Sleep Latency Test (MSLT) early in the development of narcolepsy.
- Psychiatric Disorders, Typically Depression: In psychiatric disorders, the mean sleep latency remains within the normal range.
- Movement Disorders Such as Periodic Limb Movement Disorder
- Chronic Fatigue Syndrome: Characterized by persistent fatigue that does not improve with rest or sleep.
- Medical Disorders: Chronic medical conditions, hypercapnia, and Trypanosomiasis can be differentiated through history, physical examination, and laboratory tests.
- Neurological Disorders: Including Alzheimer’s and Parkinson’s Disease.
Prognosis
Most patients diagnosed with IH usually remain stable, with approximately one in ten experiencing spontaneous improvement, a phenomenon more prevalent than in cases of narcolepsy [25]. A recent study involving a cohort of individuals with IH aged over 35 in Japan found that the only significant period associated with an increased incidence of metabolic syndrome was among several demographic variables [26].
Daytime naps exceeding an hour have been correlated with a heightened risk of stroke and hypertension, even after adjusting for cardiovascular disease and stroke risk factors. For individuals under 60, napping most days increases the likelihood of developing high blood pressure by 20% compared to those who seldom or never nap [27].
Complications
Excessive daytime sleepiness and related symptoms, such as automatic behaviors, pose a risk to oneself and others, including an elevated likelihood of motor vehicle accidents. To mitigate the potential misuse of oxybate as a “date rape” drug, its access is regulated in the United States, and it is classified under Schedule III control [28].
Prevention and Patient Education
Individuals diagnosed with IH should receive counseling regarding the risks associated with driving and operating heavy machinery. Regular follow-up appointments are necessary to evaluate any potential side effects of medications and ensure compliance with the prescribed treatment plan. In our clinical practice, we schedule follow-up visits with IH patients every six months or more frequently as needed. During these appointments, we assess for any adverse treatment effects, renew controlled substance prescriptions, address any occupational or social concerns, evaluate the effectiveness of daytime sleepiness management, and review medication adherence.
Improving Healthcare Team Outcomes
An interdisciplinary team of nurses, primary care clinicians, psychiatrists or specialists, and social workers/case managers is crucial for implementing an evidence-based approach to managing refractory daytime sleepiness and achieving favorable results. In case of treatment-related side effects or issues with adherence, timely follow-up with the patient is essential.
When medication is prescribed for idiopathic hypersomnia, pharmacists play a key role by verifying appropriate dosages, conducting medication reconciliation, and offering patient education.
Moreover, it’s imperative to counsel patients and collaborate with employers to accommodate patient schedules and ensure safety, reducing the risk of accidents and productivity issues.
All interdisciplinary team members must meticulously document patient interactions and interventions to ensure the care team is equipped with the most current and accurate information. Additionally, maintaining open lines of communication among team members facilitates prompt action in case any changes in the patient’s condition necessitate intervention. This collaborative approach across disciplines will optimize the care provided for idiopathic hypersomnia. [Level 5]
References
- Billiard M, Sonka K. Idiopathic hypersomnia. Sleep Med Rev. 2016 Oct; 29:23-33.
- Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014 Nov;146(5):1387-1394.
- Wenz E, Tafti M, Bassetti CLA. LMOD3 gene variant in familial periodic hypersomnolence. Sleep Med. 2022 Mar; 91:105-108.
- Miyagawa T, Tanaka S, Shimada M, Sakai N, Tanida K, Kotorii N, Kotorii T, Ariyoshi Y, Hashizume Y, Ogi K, Hiejima H, Kanbayashi T, Imanishi A, Ikegami A, Kamei Y, Hida A, Wada Y, Miyamoto M, Takami M, Kondo H, Tamura Y, Taniyama Y, Omata N, Mizuno T, Moriya S, Furuya H, Kato M, Kato K, Ishigooka J, Tsuruta K, Chiba S, Yamada N, Okawa M, Hirata K, Kuroda K, Kume K, Uchimura N, Kitada M, Kodama T, Inoue Y, Nishino S, Mishima K, Tokunaga K, Honda M. A rare genetic variant in the cleavage site of prepro-orexin is associated with idiopathic hypersomnia. NPJ Genom Med. 2022 Apr 12;7(1):29.
- Masunaga Y, Kagami M, Kato F, Usui T, Yonemoto T, Mishima K, Fukami M, Aoto K, Saitsu H, Ogata T. Parthenogenetic mosaicism: generation via second polar body retention and unmasking of a likely causative PER2 variant for hypersomnia. Clin Epigenetics. 2021 Apr 07;13(1):73.
- Holm A, Bang-Berthelsen CH, Knudsen S, Kornum BR, Modvig S, Jennum P, Gammeltoft S. miRNA profiles in plasma from patients with sleep disorders reveal dysregulation of miRNAs in narcolepsy and other central hypersomnia. Sleep. 2014 Sep 01;37(9):1525-33.
- Bernard-Valnet R, Frieser D, Nguyen XH, Khajavi L, Quériault C, Arthaud S, Melzi S, Fusade-Boyer M, Masson F, Zytnicki M, Saoudi A, Dauvilliers Y, Peyron C, Bauer J, Liblau RS. Influenza vaccination induces autoimmunity against orexinergic neurons in a mouse model for narcolepsy. Brain. 2022 Jun 30;145(6):2018-2030.
- Dauvilliers Y, Paquereau J, Bastuji H, Drouot X, Weil JS, Viot-Blanc V. Psychological health in central hypersomnia: the French Harmony study. J Neurol Neurosurg Psychiatry. 2009 Jun;80(6):636-41.
- Acquavella J, Mehra R, Bron M, Suomi JM, Hess GP. Prevalence of narcolepsy and other sleep disorders and frequency of diagnostic tests from 2013-2016 in insured patients actively seeking care. J Clin Sleep Med. 2020 Aug 15;16(8):1255-1263.
- Barateau L, Lopez R, Dauvilliers Y. Clinical neurophysiology of CNS hypersomnia. Handb Clin Neurol. 2019; 161:353-367.
- Mahoney CE, Cogswell A, Koralnik IJ, Scammell TE. The neurobiological basis of narcolepsy. Nat Rev Neurosci. 2019 Feb;20(2):83-93.
- Trotti LM, Ong JC, Plante DT, Friederich Murray C, King R, Bliwise DL. Disease symptomatology and response to treatment in people with idiopathic hypersomnia: initial data from the Hypersomnia Foundation registry. Sleep Med. 2020 Nov; 75:343-349.
- Vernet C, Arnulf I. Idiopathic hypersomnia with and without long sleep time: a controlled series of 75 patients. Sleep. 2009 Jun;32(6):753-9.
- Nevsimalova S, Susta M, Prihodova I, Horvat EM, Milata M, Sonka K. Idiopathic hypersomnia: a homogeneous or heterogeneous disease? Sleep Med. 2021 Apr; 80:86-91.
- Anderson KN, Pilsworth S, Sharples LD, Smith IE, Shneerson JM. Idiopathic hypersomnia: a study of 77 cases. Sleep. 2007 Oct;30(10):1274-81.
- Billiard M, Sonka K. Idiopathic Hypersomnia: Historical Account, Critical Review of Current Tests and Criteria, Diagnostic Evaluation in the Absence of Biological Markers and Robust Electrophysiological Diagnostic Criteria. Nat Sci Sleep. 2022; 14:311-322.
- Maski K, Trotti LM, Kotagal S, Robert Auger R, Rowley JA, Hashmi SD, Watson NF. Treatment of central disorders of hypersomnolence: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2021 Sep 01;17(9):1881-1893.
- Lavault S, Dauvilliers Y, Drouot X, Leu-Semenescu S, Golmard JL, Lecendreux M, Franco P, Arnulf I. Benefit and risk of modafinil in idiopathic hypersomnia vs. narcolepsy with Cataplexy. Sleep Med. 2011 Jun;12(6):550-6.
- Mayer G, Benes H, Young P, Bitterlich M, Rodenbeck A. Modafinil in the treatment of idiopathic hypersomnia without long sleep time–a randomized, double-blind, placebo-controlled study. J Sleep Res. 2015 Feb;24(1):74-81.
- Dauvilliers Y, Arnulf I, Foldvary-Schaefer N, Morse AM, Šonka K, Thorpy MJ, Mignot E, Chandler P, Parvataneni R, Black J, Sterkel A, Chen D, Skobieranda F, Bogan RK. Safety and efficacy of lower-sodium oxybate in adults with idiopathic hypersomnia: a phase 3, placebo-controlled, double-blind, randomized withdrawal study. Lancet Neurol. 2022 Jan;21(1):53-65.
- Xywav – a mixed-salt oxybate oral solution for idiopathic hypersomnia. Med Lett Drugs Ther. 2021 Dec 27;63(1640):207-208.
- Takenoshita S, Nishino S. Pharmacologic Management of Excessive Daytime Sleepiness. Sleep Med Clin. 2020 Jun;15(2):177-194.
- Leu-Semenescu S, Nittur N, Golmard JL, Arnulf I. Effects of pitolisant, a histamine H3 inverse agonist, in drug-resistant idiopathic and symptomatic hypersomnia: a chart review. Sleep Med. 2014 Jun;15(6):681-7.
- Trotti LM, Saini P, Bliwise DL, Freeman AA, Jenkins A, Rye DB. Clarithromycin in γ-aminobutyric acid-Related hypersomnolence: A randomized, crossover trial. Ann Neurol. 2015 Sep;78(3):454-65.
- Bassetti C, Aldrich MS. Idiopathic hypersomnia. A series of 42 patients. Brain. 1997 Aug;120 (Pt 8):1423-35.
- Futenma K, Takaesu Y, Nakamura M, Hayashida K, Takeuchi N, Inoue Y. Metabolic-Syndrome-Related Comorbidities in Narcolepsy Spectrum Disorders: A Preliminary Cross-Sectional Study in Japan. Int J Environ Res Public Health. 2022 May 22;19(10)
- Yang MJ, Zhang Z, Wang YJ, Li JC, Guo QL, Chen X, Wang E. Association of Nap Frequency with Hypertension or Ischemic Stroke Supported by Prospective Cohort Data and Mendelian Randomization in Predominantly Middle-Aged European Subjects. Hypertension. 2022 Sep;79(9):1962-1970.
- Dominguez A, Soca Gallego L, Parmar M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jan 17, 2023. Sodium Oxybate.
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!






