Baboon syndrome, also known as symmetrical drug-related intertriginous and flexural exanthema (SDRIFE), is a striking erythematous maculopapular rash that appears symmetrically in skin folds. This unusual condition often arises after starting a particular medication. The key to treatment is stopping the trigger and applying topical or systemic corticosteroids.
In this case, a 30-year-old man presented with odynophagia, otalgia, and fever and was prescribed amoxicillin. Soon after, he developed red, itchy lesions in the cubital fossa and inguinal regions. A trip to the emergency department (ED) led to a prescription for penicillin. However, the lesions worsened, spreading symmetrically to his axillary region, nape folds, popliteal regions, perineum, and buttocks.
Returning to the ED, he was diagnosed with baboon syndrome and treated with topical steroids, leading to clear improvement.
Content Warning: This article contains explicit medical imagery. Viewer discretion is advised.
Case Presentation
- Case of the Eruptive Antibiotic Reaction
- Patient Background: 30-year-old man with no significant medical history or known allergies.
- Initial Consultation: Presented with a 2-day history of odynophagia, otalgia, and fever.
- Prescribed Medication: Amoxicillin 1g.
- Early Reaction: Developed erythematous and pruritic lesions in the cubital fossa, then the inguinal region, within 12 hours of starting the antibiotic.
- Emergency Visit #1: Received a single dose of penicillin 1,200,000 IU; reaction initially thought to be an excipient allergy.
- Symptom Progression: Lesions worsened and spread to the axillary region. Odynophagia and fever (39.3°C) persisted.
- Emergency Visit #2: The patient was apyretic but had a reddish oropharynx, purulent tonsil spots, and widespread erythematous lesions.
- Affected Areas: Nape folds, axillas, cubital fossae, popliteal regions, perineum, and buttocks, sparing the penis and scrotum.
- Lesion Details: Serous and hemorrhagic exudate vesicles in cubital and inguinal folds, no signs of infection (Fig:1&2).
- Lab Results: Showed leucocytosis (12,600/µl), neutrophilia (9,900/µl), and elevated C-reactive protein (143 mg/l).
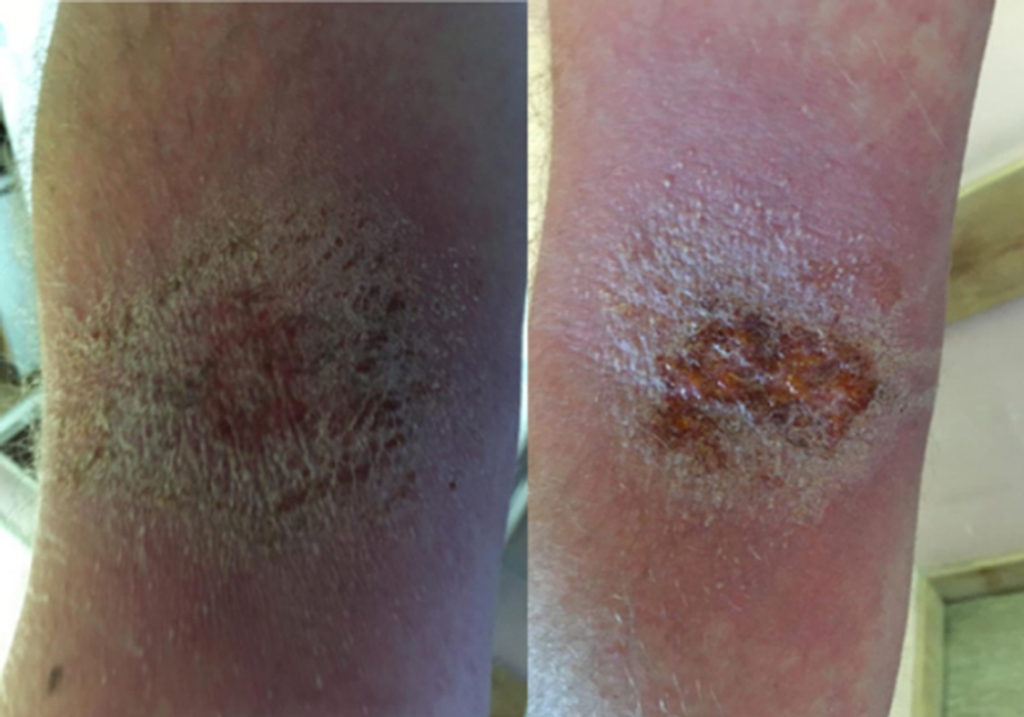 Figure 1. Rash on the cubital fossa
Figure 1. Rash on the cubital fossa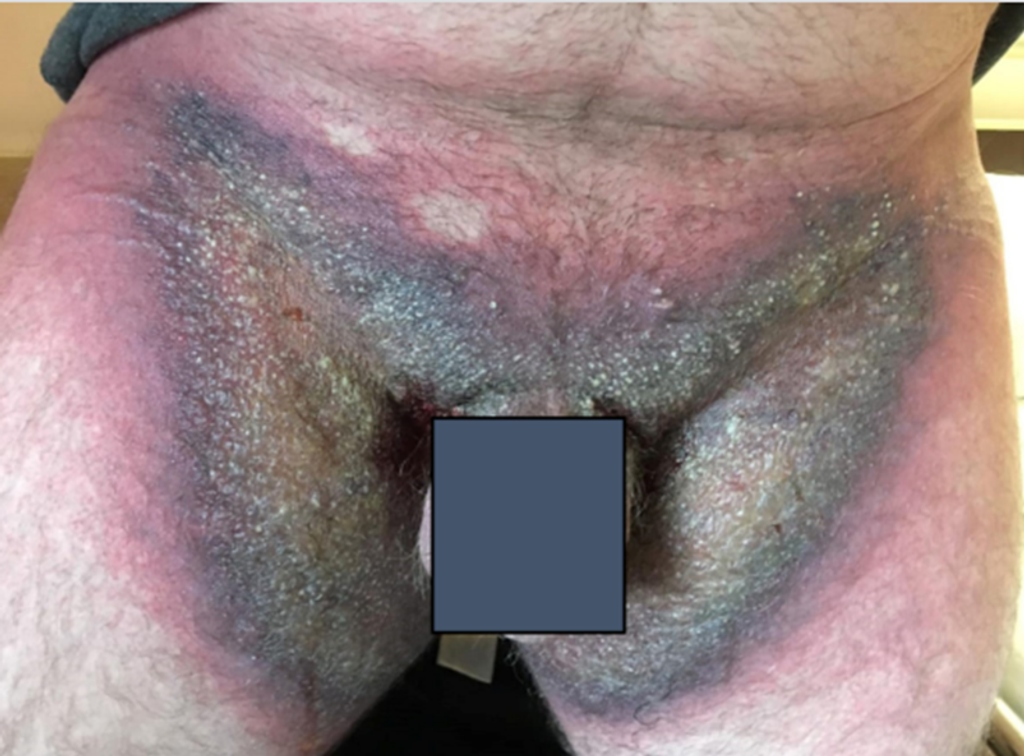 Figure 2. Rash in the inguinal folds
Figure 2. Rash in the inguinal folds
- Hospital Management and Recovery
- Medical Evaluation: Admitted to Internal Medicine; assessed by a dermatologist.
- Diagnosis: Confirmed as symmetrical drug-related intertriginous and flexural exanthema (SDRIFE), aka baboon syndrome (Fig. 3).
- Treatment Approach: Erythematous areas were treated with betamethasone, and ulcerated areas were treated with fusidic acid.
- Clinical Progress: Significant improvement was observed (Fig. 4); fever was resolved during a hospital stay.
- Discharge: Released on the fourth day post-admission.
 Figure 3. Rash on the buttocks
Figure 3. Rash on the buttocks
Discussion
Baboon syndrome, also known as SDRIFE, manifests as a distinctive rash triggered by a rare type IV hypersensitivity reaction. Its amusing moniker stems from the rash’s uncanny resemblance to a baboon’s backside [1]. Typically appearing as a red, symmetrical eruption in skin folds, the reason for its predilection in these areas remains a mystery [1, 2]. Symptoms often arise 5–14 days post-exposure to certain agents like penicillin or sooner if there’s prior sensitization [2].
Diagnosis primarily hinges on clinical observation after ruling out other potential rash causes. While some advocate for a drug-provocation test as the diagnostic gold standard, its use in the acute phase is debated [1]. Various substances, from medications such as clozapine to environmental factors like nickel, are implicated in triggering this syndrome, although penicillin is frequently involved [1, 3].
 Figure 4. Resolving rash in the inguinal folds (A) and on the cubital fossa (B)
Figure 4. Resolving rash in the inguinal folds (A) and on the cubital fossa (B)
Baboon syndrome, or SDRIFE, should be suspected when a patient presents with symmetrical erythema in major skin folds or on the buttocks, typically without systemic symptoms. Mucosal surfaces and the face are usually spared. This syndrome can manifest within hours to days upon re-exposure to the triggering agent and is more commonly observed in males [1].
The diagnostic criteria proposed by Häusermann et al. include:
(a) Exposure to a systemically administered drug, either initially or repeatedly;
(b) Distinct erythema in the gluteal area and V-shaped erythema in the inguinal/perigenital area;
(c) Involvement of at least one other skin fold;
(d) The symmetry of affected areas, and
(e) Absence of systemic symptoms [4–6].
Histologically, lesions of baboon syndrome show a superficial perivascular infiltrate of CD3 and CD4 T-cells in the dermis, occasionally with subcorneal pustules [1].
Given the widespread use of penicillin-derived antibiotics, it’s crucial to recognize associated complications, particularly dermatological, in clinical practice [2]. Allergic reactions to penicillin and its derivatives typically involve the β-lactam ring, side chains, or thiazolidine ring structures, with occasional responses to additives [6].
Treatment involves discontinuing the triggering antibiotic and administering topical or systemic corticosteroids. Symptoms typically resolve within a few days to three weeks [1, 2, 6].
Conclusion
Baboon syndrome is a rare condition that demands recognition for its clinical diagnosis and suspicion of drug-induced origins. It is typically linked to penicillin and its derivatives. While an allergy to additives was considered in this case, literature suggests such reactions are even more uncommon. Fortunately, the patient swiftly recovered with topical treatment.
References
- Lima Miranda O, Martins J, Almeida A, Formigo M, Pereira O, Rocha M, Cotter J. Symmetrical drug-related intertriginous and flexural exanthema (Baboon syndrome). EJCRIM 2021;8: doi:10.12890/2021_003029.
- Blackmur JP, Lammy S, Baring DEC. Baboon syndrome: an unusual complication arising from antibiotic treatment of tonsillitis and review of the literature. BMJ Case Rep 2013;2013: bcr2013201977. doi:10.1136/bcr-2013-201977.
- Fischbach S, Hall N, Bains S, Selvaraj V. An unusual case of worsening cellulitis: baboon syndrome or SDRIFE. BMJ Case Rep 2018;2018: bcr2018224503. doi:10.1136/bcr2018-224503.
- Liu J, Li L-F. Symmetrical drug-related intertriginous and flexural exanthema/baboon syndrome induced by traditional Chinese medicine. J Cosmet Dermatol 2021; 00:1–5. https://doi.org/10.1111/jocd.14343.
- Miyahara A, Kawashima H, Okubo Y, Hoshika A. A new proposal for a clinical-oriented subclassification of baboon syndrome and a review of baboon syndrome. Asian Pac J Allergy Immunol 2011; 29:150–160.
- Akkari H, Belhadjali H, Youssef M, Mokni S, Zili J. Baboon syndrome induced by hydroxyzine. Indian J Dermatol 2013; 58:244.
- Handisurya A, Stingl G, Wohrl S. SDRIFE (baboon syndrome) induced by penicillin. Clin Exp Dermatol 2009; 34:355–357. doi:10.1111/j.1365-2230.2008. 02911.x
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!







