Surgeons at NYU Langone Health achieve the world’s first whole eye transplant, a groundbreaking milestone in ocular transplantation. Aaron James, a high-voltage power line accident survivor, undergoes surgery for both cosmetic and functional benefits, showing promising healing and sensory progress1. This pioneering procedure opens avenues for understanding eye transplantation and advancing blindness treatments. In a retrospective study, the controversial whole-eye transplant (WET) of 1969 by Texas Medical Center (TMC) surgeon Conard Moore, MD, is reexamined. Historical reports and new materials are reviewed, exploring whether Moore performed a WET or a different operation2. The study delves into the medical and ethical factors, comparing the parameters for experimental surgery of that era to current policies.
Introduction
The world’s first whole eye transplant signifies a major leap in ocular transplantation. Aaron James, a high-voltage accident survivor, undergoes this unprecedented surgery to improve facial appearance and contribute to scientific knowledge about eye healing and potential vision restoration1. Simultaneously, a retrospective study investigates the controversial WET of 1969, raising questions about the boundaries between accepted and experimental operations and emphasizing the need for modern bioethics oversight2.
History of Eye Transplantation

Research in WET is advancing toward its application in living human recipients, but several challenges persist. Beyond surgical and neurological considerations, ethical concerns play a crucial role. These include patients’ preferences for both non-vision-restoring and vision-restoring WET, assessing risks and benefits in comparison to prosthetic alternatives, psychosocial considerations related to personal identity for potential recipients, public perceptions of whole-eye donation, implications for corneal transplantation eligibility, consent for whole-eye donation, and ethical mechanisms for allocation and distribution of WET 2. Limited studies, starting with the first vascularized composite allotransplantation (VCA) 3 in 1998, shape our understanding of WET, with amphibian regeneration studies offering insights that are not directly applicable to humans. Ocular transplants may be a viable option for form restoration in patients undergoing facial transplantation with enucleated orbits.
Historical Context
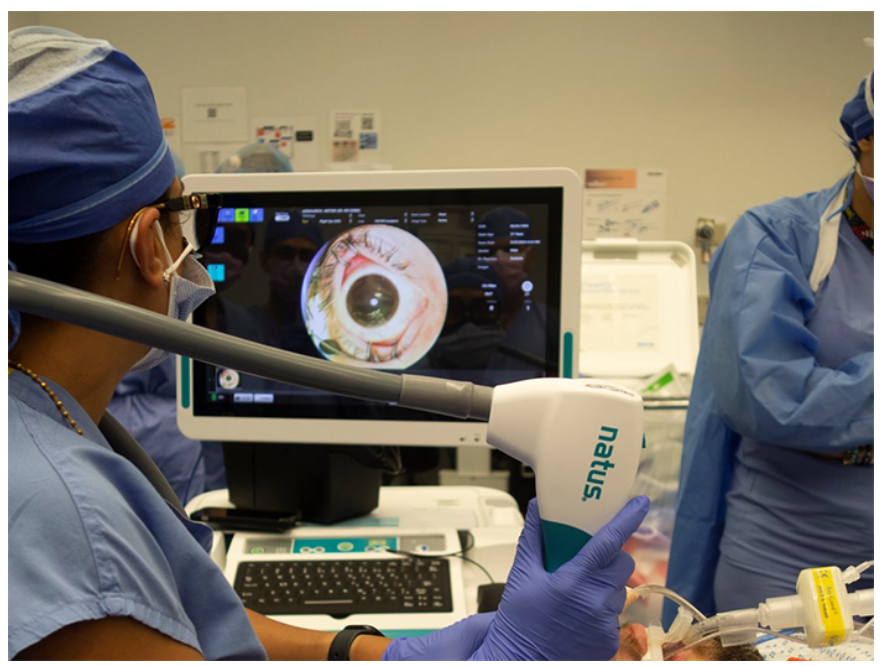
Attempts at eye transplantation date back to 1885 when Dr. Chibret replaced the eye of a 17-year-old girl with that of a rabbit, which unfortunately failed due to inadequate immunosuppression 4. In 1969, Conrad Moore claimed the transplantation of a whole eye at the Texas Medical Center but later retracted the statement 2. A significant breakthrough came in November 2023 when surgeons at NYU Langone Health achieved the first successful eye transplantation as part of a partial face transplant for Aaron James. Despite the eye displaying well-functioning blood vessels and a promising retina, it does not use the optic nerve for communication with the brain, and James has not regained sight through the eye. The lead surgeon, Eduardo D. Rodriguez, emphasized the primary goal of performing the technical operation, with adult stem cells harvested from James’s bone marrow injected into the optic nerve as part of the ongoing research for potential vision restoration 1.
Background

Aaron James’s facial injuries, resulting from a high-voltage power line accident, led to extensive damage, particularly to one eye. NYU Langone Health surgeons opt for a full eye transplant to support facial reconstruction. The success of this May surgery sparks optimism about the future of eye transplantation. Simultaneously, the reexamination of Conard Moore’s controversial 1969 WET adds historical depth, emphasizing the delicate balance between accepted and experimental surgical procedures1.
Results and Progress
Post-surgery, Aaron James exhibits positive recovery signs. While vision restoration isn’t guaranteed, the transplanted eye appears healthy, and James experiences sensory feedback. Lack of immediate complications and preserved blood flow are encouraging indicators1. This surgery offers a unique chance to study the complexities of the healing process and optic nerve repair. In the retrospective study, new evidence emerges supporting Moore’s initial claim, raising intriguing questions about surgical procedures’ accepted and experimental boundaries2.
Challenges and Future Prospects
Despite the groundbreaking success, challenges persist in regrowing the optic nerve, which is crucial for vision restoration. Ongoing brain scan analysis reveals intriguing signals from the injured optic nerve, inspiring further research. Experts acknowledge the audacity of aiming for optic nerve repair, expecting this success to drive more investigations. Simultaneously, reexamining the 1969 WET case raises questions about experimental surgeries’ historical context and ethical considerations 2.
Conclusion
The world’s first whole eye transplant marks a remarkable stride toward curing blindness. Aaron James’s case, despite challenges, provides valuable insights into transplanted eye healing 1. The retrospective study on Conard Moore’s 1969 WET adds historical depth, emphasizing the delicate balance between accepted and experimental surgical procedures 2. As we approach potentially regrowing optic nerves, this groundbreaking surgery propels ocular transplantation advancements, offering hope to those with vision-related impairments and prompting a reevaluation of historical surgical claims.
References
- Lapid N. Surgeons in New York announce world’s first eye transplant. Reuters [Internet]. 2023 Nov 9; Available from: https://www.reuters.com/business/healthcare-pharmaceuticals/surgeons-new-york-announce-worlds-first-eye-transplant-2023-11-09/
- Blodi CF. Novel Insights Into the 1969 Whole-Eye Transplant: Medical Ethics and Evolving Safety Mechanisms. American Journal of Ophthalmology. 2022 Jun;238:120–7.
- Brandacher, Gerald. Vascularized composite allotransplantation: a field is maturing. Current Opinion in Organ Transplantation 23(5):p 559-560, October 2018. | DOI: 10.1097/MOT.0000000000000574
- Psychosocial Care of End-Stage Organ Disease and Transplant Patients. Springer eBooks. 2019. DOI:10.1007/978-3-319-94914-7