Alcohol-associated liver disease (ALD) stands as the predominant cause of advanced hepatic conditions globally, often necessitating liver transplantation. The escalating prevalence of harmful alcohol consumption in the past decade has led to a rapid increase in the healthcare burden associated with ALD. The spectrum of ALD spans from early asymptomatic liver injury to advanced stages featuring decompensation and portal hypertension. Notably, patients with ALD exhibit faster progression and frequently present at an advanced stage compared to those with other liver disease etiologies. Alcohol-Associated Hepatitis (AH) represents a distinctive phenotype of advanced disease, characterized by the abrupt onset or deterioration of jaundice and acute-on-chronic liver failure, with severe cases posing a 1-month mortality risk ranging from 20% to 50%. The Model for End-Stage Liver Disease (MELD) score proves to be the most accurate tool for stratifying AH severity (a score of >20 indicates severe disease). Currently, corticosteroids stand as the sole proven therapeutic option for severe AH, demonstrating a 50%-60% survival benefit at one month.
Achieving alcohol abstinence, a pivotal factor for long-term outcomes proves challenging in ALD patients with concurrent Alcohol Use Disorder (AUD). Given the infrequent treatment of AUD in ALD patients, strategies are imperative to surmount barriers to AUD treatment in this population.
A comprehensive, multidisciplinary integrated care model involving hepatology, addiction medicine providers, and social workers is advocated to manage the dual pathologies of liver disease and AUD effectively. Liver transplantation, a definitive treatment for advanced cirrhosis, should be considered in select AH patients who are unresponsive to medical therapy and exhibit a low risk of post-transplant alcohol relapse. The Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) system was employed to evaluate the evidence and strength of recommendations in formulating this guideline, which was developed under the auspices of the American College of Gastroenterology Practice Parameters Committee.
INTRODUCTION
Alcohol-associated liver disease (ALD) constitutes a prominent contributor to preventable liver-related morbidity and mortality globally, including within the United States. The consumption of harmful levels of alcohol (defined as ≥3 drinks per day or ≥21 drinks per week in men and ≥2 drinks per day or ≥14 drinks per week in women) poses a significant risk for liver damage and ALD, often manifesting concurrently with alcohol use disorder (AUD)1,2. This pattern of alcohol use is linked to adverse social and health outcomes. The spectrum of ALD encompasses conditions ranging from steatosis and steatohepatitis to progressive fibrosis, cirrhosis, and Hepatocellular Carcinoma (HCC). Notably, it also includes the distinctive presentation of alcohol-associated hepatitis (AH), which can progress to Acute-on-Chronic Liver Failure (ACLF) in severe cases (see Figure 1).
The diagnosis of ALD necessitates the identification of chronic and harmful alcohol use, determined through patient self-report or the detection of alcohol biomarkers, along with the exclusion of other liver-affecting diseases. It is essential to recognize that harmful alcohol use may expedite the progression of other hepatic conditions, such as Metabolic Dysfunction-Associated Steatosis Liver Disease (MASLD). Individuals in the early stages of ALD may be asymptomatic, displaying features like steatosis or steatohepatitis and early-stage fibrosis. Advanced cases of ALD may present with significant fibrosis, including cirrhosis, along with complications such as ascites, hepatic encephalopathy, variceal bleeding, and HCC, or symptomatic AH featuring jaundice and ACLF 1.
Treating AUD to achieve sustained abstinence emerges as the most effective strategy to impede disease progression and enhance long-term outcomes at any stage of ALD. Liver transplantation (LT) remains a definitive therapeutic option for individuals with end-stage liver disease attributed to alcohol-associated cirrhosis and HCC.
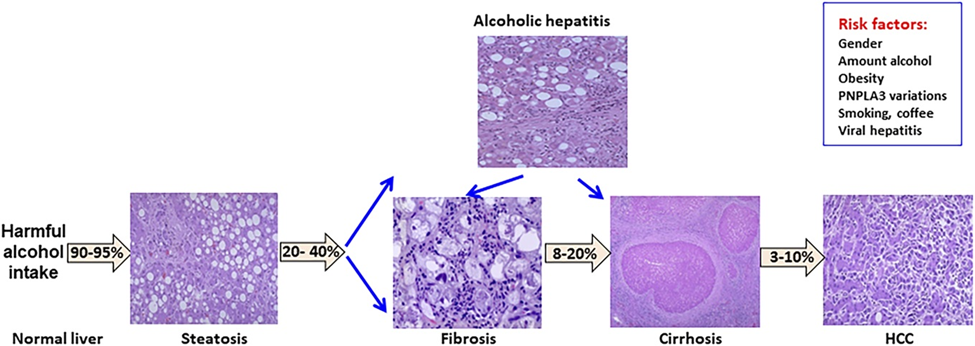
Figure 1: Disease spectrum of alcohol-associated liver disease. HCC, hepatocellular carcinoma.
Significant strides have been made in advancing our comprehension of Alcohol-Associated Liver Disease (ALD), encompassing several key aspects:
- Gaining insights into the natural history and prevalence of early ALD among individuals at risk due to harmful alcohol use or Alcohol Use Disorder (AUD).
- Observing an escalating prevalence of severe ALD forms among younger individuals, women, and specific ethnic groups, such as Hispanics and American Indians.
- Understanding the genetic and environmental factors influencing disease susceptibility and progression.
- Utilizing noninvasive techniques to assess liver fibrosis in patients with early ALD.
- Identifying individuals at high risk of disease progression.
- Establishing clinical criteria for diagnosing Alcohol-Associated Hepatitis (AH), simplifying treatment decisions, and recruitment for clinical trials.
- Recognizing the benefits of early Liver Transplantation (LT), i.e., with less than six months of alcohol abstinence, with growing acceptance and refinement of selection criteria for this salvage therapeutic option in severe AH cases.
- Emphasizes the role of multidisciplinary integrated clinical care models involving hepatology and addiction specialists to address the dual challenges of liver disease and AUD and improve long-term outcomes for ALD patients.
While significant progress has been achieved in the therapeutic pipeline for ALD and AH patients, sustained efforts are imperative for the development of effective pharmacotherapeutic options.
The Board of Trustees and Practice Parameters Committee of the American College of Gastroenterology (ACG) commissioned this practice guideline document on managing patients with ALD. The recommendations, formulated using the Patient-Intervention-Comparison-Outcome (PICO) format and Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) analysis, are summarized in (Table 1). Customizing these recommendations and guidelines based on individual patient characteristics and specific clinical scenarios in routine practice is essential. Key concepts and suggestions drawn from expert opinions and literature review are succinctly outlined in (Table 2).


The GRADE system, recommended by the A.C.G. Practice Parameters Committee, was utilized to assess the level of evidence and strength of recommendations. The strength of recommendation was categorized as strong or conditional, reflecting a consensus among the authors and considering the balance between desirable and undesirable intervention effects. The determination of the level of evidence was carried out independently by members of the GRADE team at A.C.G. (R.J.W. and B.G.S.), designated as high, moderate, low, or very low. Based on the current literature, this classification considered the confidence in the effect estimate.
EPIDEMIOLOGY AND DISEASE BURDEN
Key concept/statement
- Globally, Alcohol-Associated Liver Disease (ALD) stands as a significant contributor to advanced liver disease and liver-related mortality, a trend also observed in the United States.
- The prevalence of ALD has been on the rise since 2014, displaying an accelerated trajectory in recent years. This upward trend has led to a notable increase in healthcare and economic burdens.
- Younger adults, women, and minorities have experienced a substantial surge in Alcohol Use Disorder (AUD) and ALD. This emphasizes the importance of directing targeted prevention and treatment efforts toward these key populations.
RISK FACTORS FOR ALD
Key concept/statement
- The primary factors that contribute to the development of ALD are the quantity and duration of alcohol consumption. It is crucial to incorporate information about the potential risks of alcohol use into education programs focused on liver health.
- Individuals with pre-existing liver conditions, aside from ALD, face an elevated risk of advanced liver disease when engaging in daily alcohol consumption or binge drinking. Therefore, individuals with known liver diseases should receive counseling regarding the potential dangers associated with any level of alcohol use.
- Currently, there is insufficient data to establish a connection between binge drinking without daily heavy alcohol use and an increased susceptibility to advanced forms of ALD.

- All forms of alcohol elevate the risk of liver disease, but available data indicate that the risk might be greater with liquor compared to beer or wine.
- Genetic variations in α-1 antitrypsin, PNPLA3, TM6SF2, and MBOAT7 are linked to the risk of ALD; however, adequate data is insufficient to justify their incorporation into clinical management algorithms.
DIAGNOSIS AND TREATMENT OF AUD
Key concept/statement
- Consistent screening procedures for Alcohol Use Disorder (AUD) should be integrated into every medical interaction, spanning various clinical environments, including primary care, with a focus on conducting unbiased screening.
- Utilizing alcohol biomarkers could serve as a valuable supplement to clinical questioning and alcohol use surveys. The test selection should be customized based on the suspected timeframe of alcohol consumption.

- The assessment and management of Alcohol Withdrawal Syndrome (AWS) in individuals with Alcohol Use Disorder (AUD) and Alcohol-Related Liver Disease (ALD) should follow the Clinical Institute Withdrawal Assessment-Alcohol-revised (CIWA-Ar) protocol. Clinicians must be diligent in distinguishing AWS from hepatic encephalopathy and recognize the potential coexistence of these two conditions.
ALL DISEASE SPECTRUM
Key concept/statement
- Utilize noninvasive blood and radiological tests (NITs) to evaluate the severity of fibrosis in individuals with asymptomatic Alcohol-Related Liver Disease (ALD). Among these, the FIB-4 score, a blood-based marker, and hepatic transient elastography are recommended as the initial NITs for assessing fibrosis in individuals with ALD.
- For individuals with a history of heavy drinking who exhibit evidence of ALD identified through NITs. It is advisable to provide counseling regarding the risk of progressive liver disease and refer them to a healthcare provider with expertise in liver conditions.
- While liver biopsy is not obligatory for staging fibrosis, it may be necessary if diagnostic uncertainty persists after noninvasive assessments.
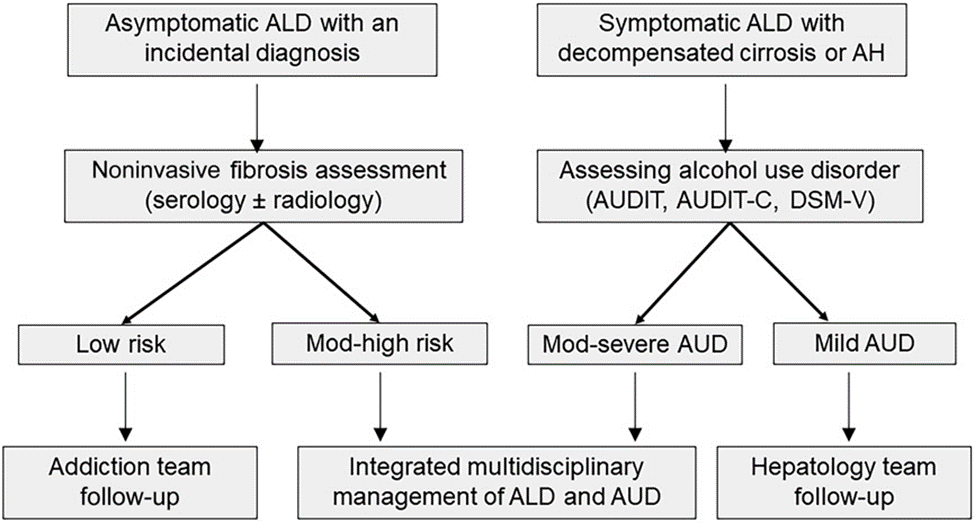
Figure 2: Integrated multidisciplinary care model for management of the dual pathology of alcohol use disorder and of alcohol-associated liver disease at any spectrum of liver disease. AH, alcohol-associated hepatitis; ALD, alcohol-associated liver disease; AUD, alcohol use disorder; AUDIT, AUD Identification Test; AUDIT-C, Alcohol Use Disorders Identification Test-Consumption; DSM-V, diagnostic and statistical manual.
- Conducting Noninvasive Tests (NITs) to screen individuals with a history of heavy drinking for the early detection of Alcohol-Related Liver Disease (ALD) proves to be a cost-effective approach.
Management of ALD
Key concept/statement
- Individuals with cirrhosis stemming from Alcohol-Related Liver Disease (ALD) should be treated in a manner consistent with those experiencing cirrhosis from alternative causes.
- Patients facing complications arising from cirrhosis related to ALD should be directed toward Liver Transplantation (LT) when deemed medically necessary.
AH
Key concept/statement
- The diagnostic criteria provided by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) serve as a valuable tool for establishing a probable diagnosis of Alcoholic Hepatitis (AH). Those meeting the criteria are eligible for corticosteroid treatment or may be considered for enrollment in clinical trials. A liver biopsy is not essential for diagnosing AH unless there are confounding factors.
- Individuals experiencing severe Alcoholic Hepatitis (AH), defined by a Model for End-Stage Liver Disease (MELD) score exceeding 20, face a high short-term mortality risk and are ideally managed through hospitalization.
- Individuals with moderate Alcoholic Hepatitis (AH), characterized by a MELD score of 20 or lower, encounter notable morbidity and mortality. Further research is required to investigate this phenotype and develop effective therapeutic approaches.
- Maintaining sustained abstinence from alcohol is linked to long-term survival following both severe and moderate cases of Alcoholic Hepatitis (AH).

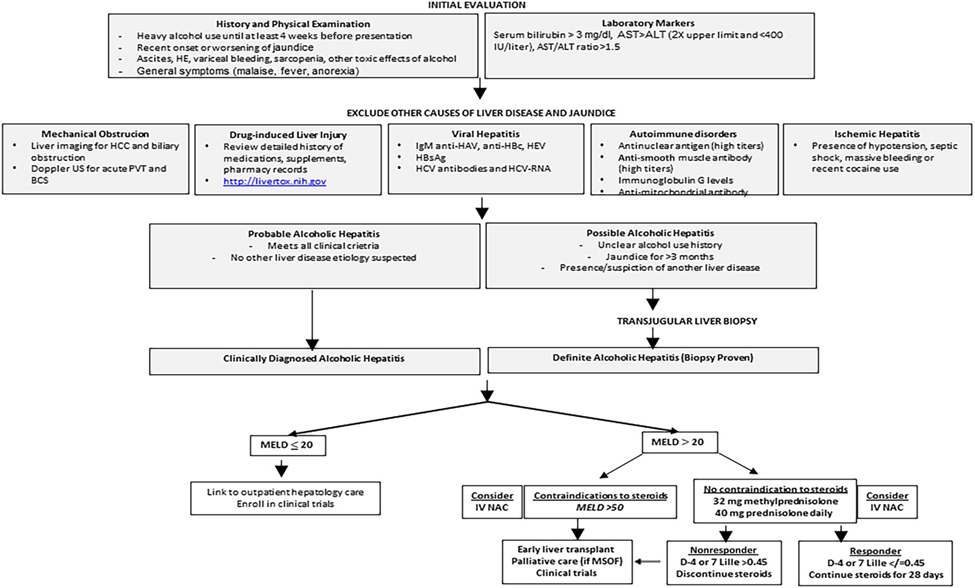
Figure 3: Algorithmic approach toward diagnosis and management of alcohol-associated hepatitis. ALT, alanine aminotransferase; AST, aspartate aminotransferase; BCS, budd chiari syndrome; HE, hepatic encephalopathy; HEV, hepatitis E virus; HCC, hepatocellular carcinoma; PVT, portal vein thrombosis.
- In cases of Alcoholic Hepatitis (AH), a MELD score exceeding 20 can serve as a means to categorize the severity of the disease, forecast the risk of short-term mortality, and inform decisions regarding the utilization of corticosteroid therapy.
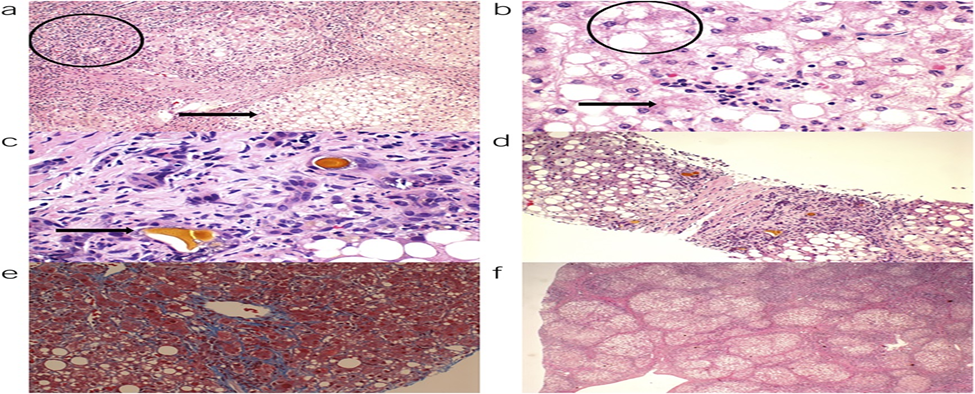
Figure 4: Histologic features of alcoholic hepatitis: (a) circle represents lobular inflammation, and arrow represents steatosis, (b) hepatocyte ballooning, (c) cholestasis with bile canalicular and hepatocyte plugging, (d) steatosis and fibrosis, (e) chicken wire and pericellular fibrosis, and (f) cirrhosis.
- For patients with Alcoholic Hepatitis (AH), it is recommended to aim for a caloric intake of 35 kcal/kg/d along with 1.2–1.5 g/kg/d of protein. Those consuming less than 21 kcal/kg/d should receive nutritional support, preferably through oral or enteral routes.
- Thiamine, vitamin B12, and zinc deficiencies are prevalent in individuals with AH and should be addressed through supplementation.
- Individuals with severe Alcoholic Hepatitis (AH) and MELD scores between 25 and 39 experience optimal outcomes with corticosteroid use. When contemplating corticosteroids for individuals with MELD scores surpassing 50, a thoughtful evaluation of risks and benefits is essential.
- The response to corticosteroid treatment can be assessed using the Lille score on either day 7 or 4. In cases where individuals exhibit a lack of response (Lille score >0.45), discontinuation of corticosteroids is recommended.
Liver Transplantation
Key concept/statement
- In cases of severe Alcoholic Hepatitis (AH), where patients are unresponsive to corticosteroids and not eligible for early Liver Transplantation (LT) due to having four or more organ failures, palliative therapy would be considered appropriate.
- The criteria for Liver Transplantation (LT) in patients with Alcohol-Related Liver Disease (ALD) should not be solely based on a predefined duration of sobriety. The transplant team’s decision-making should be informed by a thorough psychosocial assessment conducted by a social worker and an addiction specialist.
- In evaluating LT candidacy, various tools such as the Stanford Integrated Psychosocial Assessment Tool, High Risk for Alcohol Relapse Score, Michigan Alcoholism Prognostics Score, Hopkins Psychosocial Score, and Sustained Alcohol Use Posttransplant (SALT) Score may be utilized in conjunction with the assessment conducted by the addiction team.
- Individuals who have undergone Liver Transplantation (LT) should undergo monitoring for alcohol use, employing either self-report tools or alcohol biomarkers. The objective is to detect any signs early on, facilitating timely interventions to support a return to abstinence.
- For LT recipients, a multidisciplinary integrated care model is recommended. This approach aims to minimize the recurrence of alcohol use and enhance long-term outcomes.
- The initiation of alcohol use at an early stage and engaging in heavy alcohol consumption poses a risk for graft loss and long-term patient mortality. Aggressive intervention is essential to attain abstinence in these cases.
PUBLIC POLICY/PREVENTION
Key concept/statement
- The implementation of public policy interventions holds the potential to alleviate the impact of Alcohol Use Disorder (AUD) and complications associated with alcohol on the liver. These interventions should be more broadly employed to diminish alcohol-related morbidity and mortality.
RECOMMENDATIONS
- For individuals with heavy alcohol use, we strongly advise refraining from any form of tobacco consumption due to the significantly heightened risk of cirrhosis (strong recommendation, very low level of evidence).
- In individuals with obesity, a strong recommendation is made to abstain from alcohol consumption (strong recommendation, moderate level of evidence).
- To facilitate weight management and glucose control in individuals with obesity or type 2 diabetes, it is suggested to consider abstaining from alcohol use (conditional recommendation, very low level of evidence).
- For individuals undergoing gastric bypass surgery or with a history thereof, a strong recommendation is made to steer clear of heavy alcohol use (strong recommendation, very low level of evidence).
- In patients dealing with chronic HCV infection, it is strongly recommended to avoid alcohol consumption (strong recommendation, high level of evidence).
- For patients coping with chronic HBV infection, a strong recommendation is made to refrain from alcohol consumption (strong recommendation, low level of evidence).
- For adults undergoing alcohol use screening, we strongly advocate the utilization of concise screening instruments, such as the Alcohol Use Disorders Identification Test-Consumption tool (strong recommendation, high-quality evidence).
- For individuals with both Alcohol-Related Liver Disease (ALD) and Alcohol Use Disorder (AUD), it is strongly recommended to integrate brief motivational interventions into their clinical care (strong recommendation, low-quality evidence).
- For individuals with compensated Alcohol-Related Liver Disease (ALD), it is strongly recommended to consider baclofen as a treatment option for Alcohol Use Disorder (AUD) (strong recommendation, moderate level of evidence).
- In individuals with compensated ALD, the use of acamprosate or naltrexone is suggested as an option for treating AUD (conditional recommendation, very low level of evidence).
- For individuals with compensated ALD, the use of gabapentin or topiramate is suggested as an option for treating AUD (conditional recommendation, very low level of evidence).
- Disulfiram should be avoided in the treatment of AUD across all stages of ALD (conditional recommendation, very low level of evidence).
- For individuals with Alcohol-Related Liver Disease (ALD) experiencing severe Alcohol Withdrawal Syndrome (AWS), it is strongly recommended to exercise caution when considering benzodiazepines as the treatment of choice. Careful monitoring is advised due to the potential of benzodiazepines to trigger or worsen hepatic encephalopathy (strong recommendation, moderate level of evidence).
- In individuals with Alcohol-Related Liver Disease (ALD), we strongly recommend providing integrated multidisciplinary care models that include behavioral or pharmacotherapy for the treatment of Alcohol Use Disorder (AUD) (strong recommendation, low level of evidence).
- For hospitalized patients experiencing severe Alcoholic Hepatitis (AH), we strongly advise not universally administering prophylactic antibiotics (strong recommendation, moderate level of evidence).
- For individuals with Alcoholic Hepatitis (AH) who are malnourished or unable to fulfill their caloric needs solely through oral nutrition, we recommend incorporating oral nutritional supplements. If patients still struggle to meet their caloric requirements even with oral supplements, we strongly recommend enteral nutrition support (strong recommendation, moderate level of evidence).
- For individuals experiencing severe Alcoholic Hepatitis (AH) with a Model for End-Stage Liver Disease (MELD) score exceeding 20, we strongly recommend initiating corticosteroid therapy if no contraindications are present (strong recommendation, moderate level of evidence).
- The utilization of Pentoxifylline (PTX) is strongly discouraged for individuals with severe Alcoholic Hepatitis (AH) (strong recommendation, moderate level of evidence).
- The role of granulocyte colony-stimulating factor (G-CSF) and microbiome-based therapies in treating severe AH is not well-established due to insufficient data (conditional recommendation, moderate level of evidence).
- It is strongly recommended to use Intravenous N-acetylcysteine as an adjuvant to corticosteroids in patients with severe AH (strong recommendation, moderate level of evidence).
CONCLUSIONS AND PROSPECTS
The healthcare burdens stemming from Alcohol Use Disorder (AUD) and Alcohol-Associated Liver Disease (ALD) are substantial, both in the United States and globally, with a noticeable uptick in recent years. Providers across all clinical domains must be equipped to manage this expanding patient population. Individuals with ALD are often present at an advanced stage, receive limited attention for AUD treatment, and have few effective therapies targeting their liver disease. A glimmer of hope is on the horizon, with continued and escalating interest from researchers and funding organizations, notably the NIAAA, offering the potential to address knowledge gaps and unmet clinical needs in ALD (refer to Table 6). Research efforts should be concentrated on policy initiatives aimed at reducing alcohol use, implementing multidisciplinary care strategies for the concurrent diagnoses of AUD and ALD, and refining Liver Transplantation (LT) algorithms for patients with severe Alcohol-Associated Hepatitis (AH).
References
- Joplin, Loretta L. MD, PhD1, *; Singal, Ashwani K. MD, MS, FACG2, *; Bataller, Ramon MD, Ph.D., FACG3; Wong, Robert J. MD, MS, FACG4; Sauer, Bryan G. MD, MSc, FACG5; Terrault, Norah A. MD, MPH, FACG6; Shah, Vijay H. MD, FACG7. ACG Clinical Guideline: Alcohol-Associated Liver Disease. The American Journal of Gastroenterology 119(1): p 30-54, January 2024. | DOI: 10.14309/ajg.0000000000002572
- Singal A, Mathurin P. Diagnosis and treatment of alcohol-associated liver disease: A review. JAMA 2021;326(2):165–76.
- Bataller R, Arab JP, Shah VH. Alcohol-associated hepatitis. N Engl J Med 2022;387(26):2436–48.
- Yoon Y-H, Chen CM, Yi H-y. Liver Cirrhosis Mortality in the United States: National, State, and Regional Trends, 2000–2011. National Institutes of Health: Arlington, VA, 2014. Report no.: surveillance report #100, December.
- Organization WWH. Alcohol 2022. (https://www.who.int/news-room/fact-sheets/detail/alcohol)
- Chen CM, Yoon Y-H. Liver cirrhosis mortality in the United States: national, state, and regional trends, 2000–2019. National Institutes of Health: Sterling, VA, 2022. February.
- Philip G, Hookey L, Richardson H, et al. Alcohol-associated liver disease is now the most common indication for liver transplant waitlisting among young American adults. Transplantation 2022;106(10):2000–5.
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!






