Two unique cases, one male and one female, presented with isolated perineal soft tissue injuries, including a rare condition known as Posterior Anorectal Detachment. Remarkably, both had a detached anorectum from the coccyx and sacrum, yet the rectal lumen and sphincter remained intact. Neither patient suffered a pelvic fracture, nor was the bladder or urethra compromised. A temporary colostomy was performed for each, allowing the perineal wounds to heal naturally. In the end, both patients were highly satisfied with their recovery.
Introduction to Blunt Perineal Trauma
The perineum, a diamond-shaped area at the pelvic outlet, is framed by the pubic symphysis in the front and the coccyx in the back and houses the levator ani and coccygeus muscles [1]. Injuries to this region and the lower genitourinary tract are typically acute. Research reveals those penetrating injuries, like gunshot wounds and stabbings, account for 35% of cases, while the remaining 65% stem from blunt trauma due to falls and car accidents [2]. The cases featured in this report are of the blunt trauma variety.
Blunt trauma perineal injuries are exceptionally rare, with an incidence of just 0.1% and a male-to-female ratio of 85:15 [3]. Teixeira et al. found a 36% mortality rate for such injuries, underscoring their severity [4]. These injuries are often linked with pelvic fractures, which necessitate complex repair procedures [5]. Diagnosing blunt perineal trauma varies based on the affected structures, and treatment generally involves a multidisciplinary approach, including colostomies, bladder catheters, suprapubic cystotomies, and nephrostomies [6].
In this report, we explore two cases of blunt trauma that led to perineal injuries without accompanying fractures.
Case Presentation: Posterior Anorectal Detachment
Case 1
- Patient Information:
- Age/Sex: 29-year-old male
- Incident: Car accident; a 5-ton water tanker’s wheel rolled over his lower body while he was stepping into a car.
- Initial Assessment:
- Glasgow Coma Scale (GCS): 15
- Pulse Rate: 80 beats per minute
- Blood Pressure: 90/60 mmHg
- Findings:
- Profuse bleeding from perineum injury
- X-rays showed no skull, cervical spine, or pelvic fractures
- Urinary catheterization performed without difficulty; no hematuria
- Abdominal ultrasound revealed no internal bleeding
- Immediate Action: Fluid and blood replacement; patient moved to the operating theatre for further assessment
Operative Findings and Procedure
- Preoperative Findings:
- Position: Lithotomy
- Observation:
- Anterior displacement of the anus with a circular skin defect around the area
- Anus appeared normal with a remaining 1 cm (about 0.39 in) of intact perianal skin
- Examinations: Digital and proctoscopy exams showed an intact anorectum and surrounding sphincters.
- Wound Exploration:
- Complete disruption of the posterior pelvic floor
- Lateral extensions into both gluteal regions and right thigh
- A hand could be passed behind the rectum into the sacral promontory
- Management:
- Bleeding: Extensive venous bleeding; no major arterial tears
- Treatment:
- Insertion of multiple packs and partial closure of the skin defect
- Small incision for defunctioning sigmoid colostomy
- No intra-abdominal bleeding
- Outcome:
- Packs removed two days later without complications
- 22 units of blood were administered within the first 48 hours (about 2 days).
- Figures:
- Figures 1 and 2 illustrate the injury site before and after treatment, respectively.
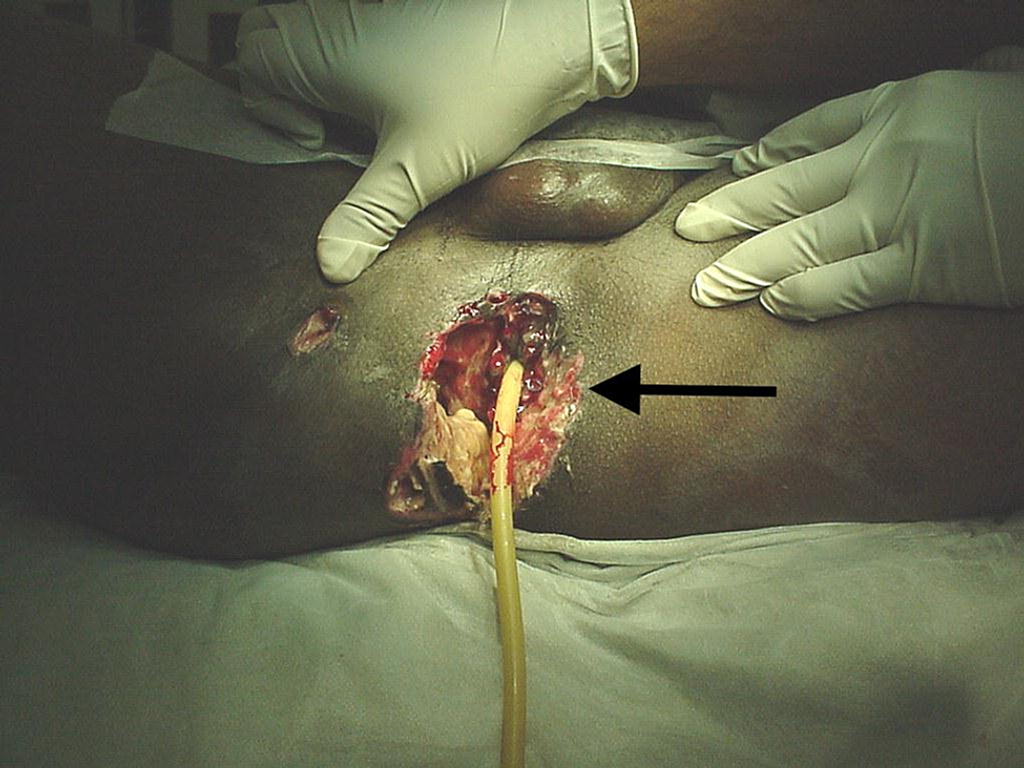 Figure 1: Injury site for Case 1 prior to treatment.
Figure 1: Injury site for Case 1 prior to treatment. Figure 1: Injury site for Case 1 post-treatment.
Figure 1: Injury site for Case 1 post-treatment.
Follow-Up and Recovery
- Ongoing Examinations:
- Frequency: Continuous follow-up over several months
- Procedures: Seven examinations under anesthesia
- Wound Management:
- Initial Issues:
- The skin is not fully closed at the site of the procedure.
- The decision was made not to reposition the anorectum further posteriorly; the wound was left open.
- Initial Treatment:
- Infection of deep injury recess found
- Debridement and daily cleaning with Betadine were performed.
- Subsequent Treatment:
- Transition to saline dressings as wound cleanliness improved
- Healing occurs by granulation.
- Wound Progress:
- Size Reduction: The defect reduced to 4 x 2 cm after four months
- Wound Contraction: Wound contracted towards the coccyx
- Anus Condition: Felt normal on digital examination, with good sphincter tone and squeeze
- Physiological Testing:
- Sphincter Function:
- Manometry Results: Resting sphincter pressure around 30 cmH2O; increased squeeze pressure due to puborectalis and gluteal muscle contraction.
- Sensation: Presence of rectal sensation noted but not quantified
- Defecography:
- Normal anorectum displaced towards the pubic bone.
- Ability to evacuate barium paste; no abnormal descent of the rectum during straining
- The anorectal angle did not widen during straining at 90°.
- Post-Surgical Outcome:
- Colostomy Closure: Completed five months after surgery
- Defecation: Normal defecation achieved without major or minor incontinence
- Patient Feedback: Satisfactory defecation and micturition; no incontinence reported during follow-up visits.
Case 2
- Patient Information: A 44-year-old female involved in a car accident was ejected from the vehicle, landing on her buttocks on a hard rock.
- Initial Hospital Findings: At the district hospital, the patient was found to have a partial laceration of the posterior perineum surrounding an intact anorectum. No injuries were noted to the bladder, urethra, or pelvis.
- Intervention: A sigmoid colostomy was performed.
- Transfer: The patient was transferred to a tertiary hospital for further care.
- Examination at Tertiary Hospital:
- Wound Assessment:
- Crescent-shaped wound surrounding the anus from the three to nine o’clock position.
- The anus is displaced anteriorly toward the vagina.
- Examination Findings: Digital and proctoscopy examinations confirmed an intact anorectum and surrounding sphincters.
- Progress and Management
- Conservative Management: The patient received identical conservative management to a previously mentioned case.
- Support System: Discharged earlier due to adequate support from her daughter, who had nursing experience.
- Wound Care
- The wound was clean and in the proliferation stage of healing.
- The patient was instructed to perform daily irrigation using handheld bidets.
- Follow-Up:
- Scheduled every three weeks, which the patient attended punctually.
- After five months, the wound was reduced to a superficial size of 1 x 2 cm and there were no infections.
- Follow-Up Findings
- Defecation Portogram Results:
- Anteriorly displaced anus with an anorectal angle of 70°, widening to 90° upon straining.
- Incomplete evacuation was observed, but no atypical rectal descent.
- The patient reported complete evacuation in the toilet after the examination.
- Post-Injury Outcome
- Seven Months Post-Injury:
- A Colostomy closure was performed.
- Five days post-closure, the patient reported normal bowel movements with no incontinence.
- The patient was subsequently discharged.
- Fifteen Months Post-Injury:
- Complete wound healing was noted with adequate defecation.
- The patient reported occasional use of glycerin suppositories.
- No fecal impaction was observed due to the treatment regimen.
- Visual Documentation
- Figures 3 & 4: Illustrate the site of injury before and after treatment, respectively.
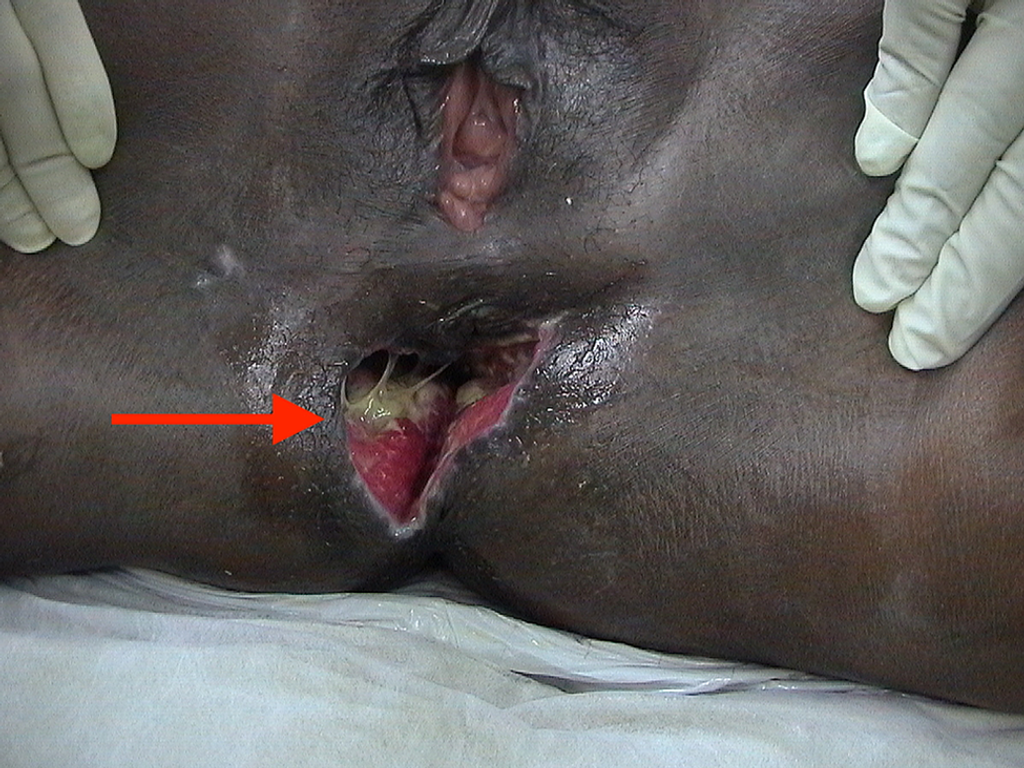
Figure 3: Site of injury of Case 2 before treatment.
Figure 4: Site of injury of Case 2 after treatment.
- Figures 3 & 4: Illustrate the site of injury before and after treatment, respectively.
Discussion
Extent of Injuries
In both cases, the injuries were marked by superficial perineal tears and significant damage to the underlying muscles. Notably, the superficial injuries involved skin tears without any actual skin loss, with the anus displaced anteriorly toward the pubic area.
- Case 1: The perineal skin was completely detached from the surrounding skin around the anus, leaving the anus deeply retracted and isolated within the subcutaneous fat layer.
- Case 2: The skin separation formed a crescent-shaped laceration at the posterior end of the perineum, with the anus remaining anteriorly connected to the skin of the perineal body.
Both cases exhibited deeper injuries involving the detachment of the pubococcygeus, iliococcygeus, and coccygeus muscles from their distal attachments. This detachment caused the anus to shift forward as the anococcygeal raphe and puborectalis muscle contracted the anorectum toward the pubis. Venous hemorrhaging in both cases resulted from blunt force trauma, which stripped the rectum from the presacral fascia, injuring the fascia and underlying veins that supply the perineum.
- Case 1 Additional Details: The first patient also experienced further separations into the right and left gluteal regions, with additional detachments extending 10-15 centimeters into the right thigh. Despite these separations, no muscle damage was noted, and it was determined that the injury involved the dissociation of interfacial planes and disruption of venous drainage. There was also a detachment of the levator ani from its insertion into the obturator internus fascia, opening the retrorectal space to the level of the pelvic peritoneum. The extent of damage to the splanchnic nerves remained undetermined.
Notably, both cases were free of internal organ injuries and bony pelvic fractures despite the severity of the trauma.
Mechanism of Injury
- Case 1: The patient described being crushed in the lower body by the weight of two rear tires passing over him. Remarkably, the injury could have been far worse if the tires had rolled over the front or side of the pelvis, likely causing fractures by compressing the ileum. However, if he had been lying face down, the soft tissues of the buttocks and perineum might have absorbed the vehicle’s weight, potentially compressing the anus and levator ani upward into the abdomen. When the pressure was released, the pelvic diaphragm might have snapped back into place, creating significant negative pressure. The resulting tissue separation likely occurred either from the initial compression or the sudden decompression.
- Case 2: The second patient described how her buttock landed directly on a rock after being thrown from a car. Given her moderate obesity (>100 kg), the fall may have compressed the pelvic diaphragm similarly to Case 1, with the soft tissues absorbing the impact and preventing pelvic fractures. Therefore, the tissue separation in this case was likely due to compression rather than decompression.
Plan of Management
A thorough visual and manual examination was conducted to assess the extent of pelvic floor disruption in both cases. No repairable tissue was identified.
- Case 1: The bleeding was so severe that controlling it became the top priority. Attempts were made to reposition the anus and close the skin defect, but they were unsuccessful. Given that the internal and external sphincters remained intact, and both the puborectalis muscle and anorectal tube were undisturbed, a conservative management approach was adopted. A sigmoid loop colostomy was performed for fecal diversion, with no attempts to repair the disrupted muscles or relocate the anus posteriorly. The skin was left open, with daily dressings applied until the wound closed. This patient’s large and initially infected wound required hospitalization for proper care.
- Case 2: Similarly, conservative management was chosen, with the skin left open and daily irrigation with water performed at home. Since the wound was clean, this simpler approach proved both effective and sufficient for healing.
Assessment of the Final Outcome
Both patients regained normal rectal function without incontinence and expressed satisfaction with the results after two years and 15 months, respectively. Despite their anatomical displacement, they maintained continence of feces, mucus, and gas, thanks to the intact sphincter mechanism and puborectalis sling. While there’s no current information on sexual function, the first patient married and conceived a child six months after the injury, while the second patient, a widow, reported no issues. The urinary bladder and voiding mechanisms also functioned normally in both cases.
Although there’s a long-term risk of perineal hernia, rectal intussusception, or prolapse, no such complications have been observed to date.
Conclusions
This case report outlines an approach to managing traumatic perineal injuries. A deep understanding of perineal anatomy and the patient’s hemodynamic stability is crucial in selecting the right treatment method. For patients with blunt soft tissue injuries to the perineum, without visceral or bony damage, management typically involves controlling bleeding, performing fecal diversion, and allowing the open wound to heal with simple dressings or cleansing. Full continence is generally expected to return within four to six months post-injury.
References
- Allawati M, Al Qubtan M, Logman T, et al. (November 09, 2021) Posterior Detachment of the Anorectum Following Blunt Trauma to the Perineum. Cureus 13(11): e19389. doi:10.7759/cureus.19389.
- Choe J, Wortman JR, Sodickson AD, Khurana B, Uyeda JW: Imaging of acute conditions of the perineum. Radiographics. 2018, 38:1111-30. 10.1148/rg.2018170151.
- Paparel P, N’Diaye A, Laumon B, Caillot JL, Perrin P, Ruffion A: The epidemiology of trauma of the genitourinary system after traffic accidents: analysis of a register of over 43,000 victims. BJU Int. 2006, 97:338-41. 10.1111/j.1464-410X.2006. 05900.x
- Petrone P, Inaba K, Wasserberg N, et al.: Perineal injuries at a large urban trauma center: injury patterns and outcomes. Am Surg. 2009, 75:317-20.
- Teixeira FJR Jr, do Couto Netto SD, Collete e Silva FS, et al.: Complex perineal injuries in blunt trauma patients: the value of a damage control approach. Panam J Trauma Crit Care Emerg Surg. 2015, 4:87-95. 10.5005/jp-journals-10030-1122.
- Wei R, Cao X, Tu D: Clinical treatment of open pelvic fractures associated with perineal injury. (Article in Chinese). Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2012, 26:550-3.
- Petrone P, Rodríguez Velandia W, Dziaková J, Marini CP: Treatment of complex perineal trauma. A review of the literature. Cir Esp. 2016, 94:313-22. 10.1016/j.cireng.2016.07.002
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia.
Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!







