In the bustling city of Changchun, China, a 26-year-old woman presented with a perplexing medical conundrum of bladder migration. For five years, she had endured frequent urination, hematuria, and persistent abdominal pain. Despite various treatments, her symptoms persisted, leaving her and her doctors at a loss. Her medical history revealed a critical detail: six years prior, she had an intrauterine device (IUD) inserted for contraception.
In 2012, while using the IUD, she became pregnant and delivered her baby via cesarean section. During the surgery, no signs of the IUD were found, leading doctors to surmise that it might have been embedded in the uterine wall. Subsequently, a second IUD was placed post-C-section. Despite its efficacy as a contraceptive, the IUD had not prevented her pregnancy, likely due to its displacement from the uterus.
When her bladder symptoms failed to improve, doctors at The First Hospital of Jilin University conducted a pelvic X-ray. The results were startling: the “missing” IUD had not only perforated the uterine wall but had migrated into the bladder. Furthermore, she still had the second IUD correctly placed in her uterus.
IUD Migration and Perforation: A Rare but Significant Risk
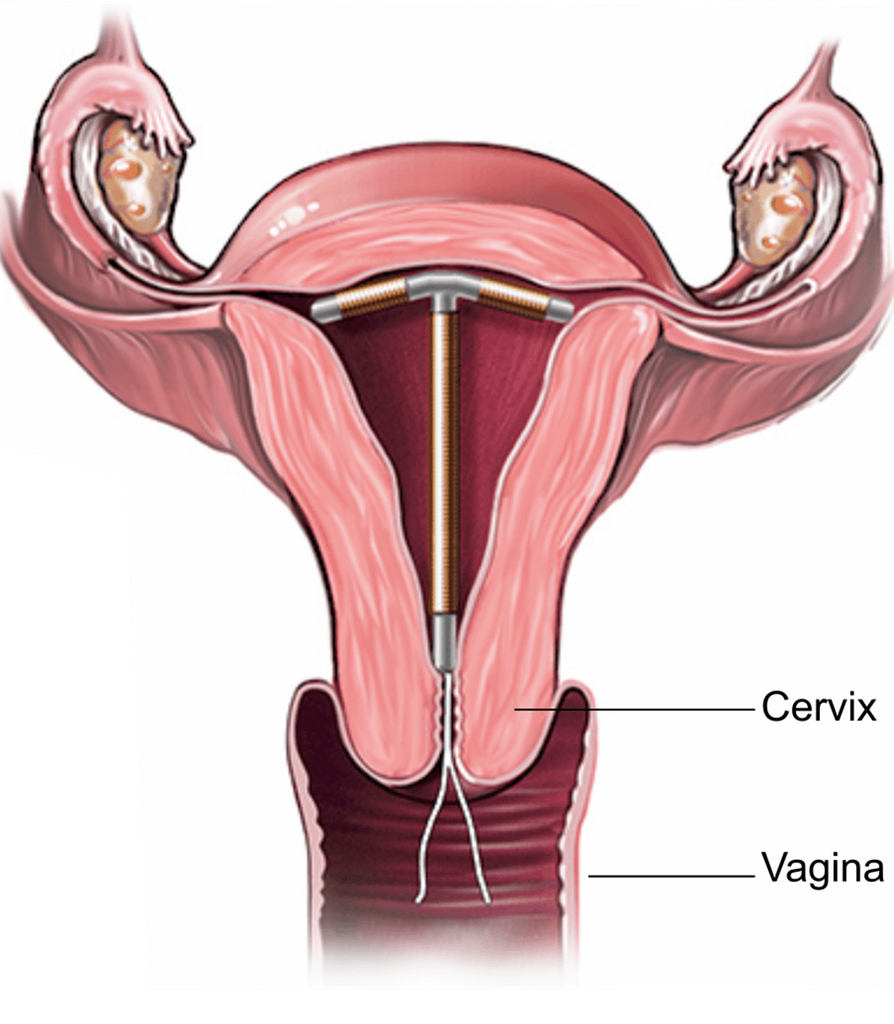
IUDs are a widely used form of long-acting, reversible contraception. They boast a high efficacy rate, with less than 1% of users experiencing pregnancy annually. However, they are not without risks. Uterine perforation by an IUD is a rare complication, occurring in about 1 in 1,000 cases.
When perforation occurs, the IUD can migrate to various abdominal or pelvic cavity parts.
The phenomenon of IUD migration to the bladder is particularly rare but has been documented. According to a 2016 report from Greece, at least 40 cases of IUD migration to the bladder have been reported in the past decade. The symptoms resulting from such migration often include chronic urinary issues, which can significantly impact the patient’s quality of life.
Mechanisms of IUD Migration
Perforation typically occurs during IUD insertion. However, in this patient’s case, the uterine contractions from pregnancy likely facilitated the IUD’s displacement. Once free from the uterine confines, the IUD migrated through the pelvic cavity, eventually perforating the bladder. Interestingly, the bladder perforation healed spontaneously, leaving behind the foreign body that caused persistent symptoms.
Bladder Migration: Diagnosis and Management
The diagnosis of a migrating IUD often requires a high index of suspicion, especially when a patient presents with a history of IUD use and unexplained symptoms. Imaging studies such as X-rays, ultrasound, or CT scans can confirm the presence and location of the IUD. In this case, the pelvic X-ray was pivotal in identifying the misplaced IUD.
Management involves carefully removing the migrated IUD to alleviate symptoms and prevent further complications. In this patient’s case, the IUD was successfully removed from the bladder without subsequent issues. Her symptoms resolved post-removal, underscoring the importance of timely intervention.
Clinical Implications
This case underscores several critical points for clinical practice:
- Vigilance for Missing IUDs: Further investigation is warranted when an IUD is not visualized during routine examinations or procedures. A “missing” IUD should prompt imaging studies to determine its location and prevent potential complications.
- Prompt Removal: An IUD found outside the uterus should be removed promptly to avoid chronic symptoms and further tissue damage.
- Patient Education: Educating patients on the signs of IUD displacement and the importance of follow-up can aid in the early detection and management of complications.
- Multidisciplinary Approach: Collaboration among gynecologists, radiologists, and urologists is crucial in managing complex cases involving migrated IUDs.
Conclusion
The case of the migrating IUD serves as a poignant reminder of the potential complications associated with contraceptive devices. While rare, IUD migration can lead to significant morbidity, as evidenced by the chronic urinary symptoms experienced by the patient in this case. This report highlights the importance of thorough investigation, prompt intervention, and patient education to ensure IUDs’ safe and effective use in clinical practice. For healthcare providers, maintaining a high index of suspicion and employing a multidisciplinary approach can mitigate risks and enhance patient outcomes.
Disclaimer Statement: This information is from a third-party health news channel. The opinions expressed here belong to the respective authors/entities and do not reflect the views of Docquity. Docquity does not assure, endorse, or vouch for any of the content and bears no responsibility for it in any way. It is essential to take all necessary steps to ensure the information and content provided are accurate, current, and verified. Docquity disclaims any express or implied warranties related to the report and its contents.
References
- Woman’s ‘Missing’ IUD Turns Up in Her Bladder [Internet]. Accessed on July 18, 2024. Available at: https://www.livescience.com/60735-woman-missing-iud-bladder.html#:~:text=In%20the%20woman’s%20case%2C%20the,chronic%20urinary%20symptoms%2C%20they%20said.
- Aydogdu O, Pulat H. Asymptomatic far-migration of an intrauterine device into the abdominal cavity: A rare entity. Can Urol Assoc J. 2012 Jun;6(3): E134-6. Doi: 10.5489/cuaj.11100. PMID: 22709887; PMCID: PMC3377742.
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!







