Although the multiple sleep latency test (MSLT) is the primary method for diagnosing narcolepsy type 1 by objectively measuring daytime sleepiness, its efficacy in evaluating non-cataplectic central disorders of hypersomnolence remains uncertain. Nonetheless, it remains the predominant diagnostic tool for patients suspected of these conditions. Roughly 30% to 40% of individuals with idiopathic hypersomnia exhibit normal MSLT results, often resulting in a dismissal of their sleepiness as unrelated to a sleep disorder.
Nancy Foldvary-Schaefer, DO, MS, Director of the Sleep Disorders Research Center, highlights the frustration of patients with severe hypersomnolence who undergo multiple inconclusive MSLTs only to be informed that their issue is psychological, medication-related, or due to another medical condition. This leaves them with limited options for further assistance. Dr. Foldvary-Schaefer advocates for broader recognition of alternative diagnostic methods for specific patient groups in the United States, such as an extended polysomnography protocol. She emphasizes these points during her presentations at medical conferences, often supplementing her arguments with case studies, as outlined below, following a brief overview of idiopathic hypersomnia.

Idiopathic Hypersomnia Patient Presentation
A woman in her late 20s presents to the Sleep Disorders Center complaining of excessive daytime sleepiness, sleep inertia, rare sleep-related hallucinations, and brain fog. Her medical history includes hypothyroidism managed with levothyroxine and a single childhood seizure.
Diagnostic History
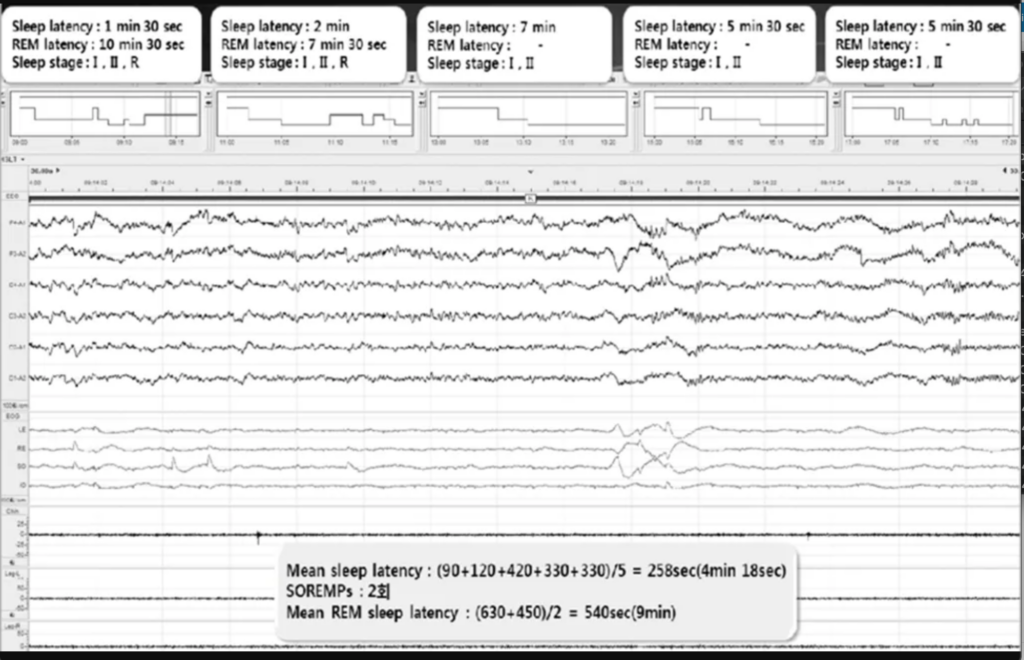
The patient underwent multiple polysomnography (PSG) followed by multiple sleep latency tests (MSLT) starting in adolescence. Results were inconsistent with hypersomnia; however, her anxiety in the testing environment may have influenced outcomes. Notably, she did not exhibit sleep-onset rapid eye movement (REM) periods indicative of narcolepsy.
Current Assessment
Actigraphy demonstrated an average sleep duration of 8.7 hours with an appropriate circadian rhythm, ruling out delayed sleep phase disorder. Given persistent symptoms and inconclusive prior testing, a 32-hour PSG bed-rest protocol was recommended.
Diagnostic Procedure
The extended PSG study revealed a total sleep time of 19.25 hours, exceeding the threshold for idiopathic hypersomnia diagnosis. Additionally, primary snoring was noted, with normal apnea-hypopnea index and oxygen levels.
Treatment Initiation
The patient was started on lower-sodium oxybate. Subsequent improvement in social and work functioning was noted by family members, describing the change as “remarkable.”
Key Considerations and Takeaways
- MSLT’s Limitations: The diagnostic value of MSLT beyond narcolepsy type 1 is questioned, underscoring the need for alternative diagnostic tools such as wrist actigraphy and the Psychomotor Vigilance Test.
- Clinical Features in Diagnosis: Clinical phenotypes, such as an unrelenting need for sleep without feeling rested, should play a central role in diagnosis. Unlike narcolepsy type 1, idiopathic hypersomnia lacks cataplexy and abrupt daytime sleep episodes.
- Role of Extended PSG: Validated for idiopathic hypersomnia, extended PSG should be considered for select cases despite current underutilization in the U.S.
- Availability of Treatment: Effective treatment options, including FDA-approved medications like lower-sodium oxybate, underscore the importance of identifying idiopathic hypersomnia.
Ongoing Research and Future Prospects
Ongoing clinical trials, such as evaluating pitolisant for idiopathic hypersomnia, hold promise for expanding treatment options. Additionally, research efforts leveraging large datasets and machine learning aim to define complex sleep disorders better and identify biomarkers for targeted therapies.
Conclusion
Comprehensive evaluation, utilizing both clinical assessment and appropriate diagnostic tools like extended PSG, is essential for accurately diagnosing and managing idiopathic hypersomnia. Integration of evolving research findings will further enhance diagnostic precision and therapeutic outcomes for patients with sleep disorders.
Reference
- Case Study: Extended Polysomnography Confirms an Idiopathic Hypersomnia Diagnosis [Internet]. Cleveland Clinic (Accessed on March 19, 2024). Available from: https://consultqd.clevelandclinic.org/case-study-extended-polysomnography-confirms-an-idiopathic-hypersomnia-diagnosis
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!