Fish Odor Syndrome (FOS), or Trimethylaminuria, is a condition where patients emit a strong smell similar to rotting fish, causing significant psychological challenges. This condition typically stems from an inherited deficiency in flavin monooxygenase 3, a vital enzyme responsible for metabolizing trimethylamine, the compound accountable for the malodorous scent. Despite its rarity, recent research suggests that the diagnosis of this disorder may frequently be overlooked. It is imperative to recognize this condition due to the availability of reliable diagnostic tests and its potential profound psychosocial impact. At the same time, there is no definitive cure; various straightforward treatment approaches can greatly enhance the quality of life for affected individuals. This article aims to explore the literature, particularly emphasizing the psychosocial implications and treatment modalities associated with Trimethylaminuria.
Key Points
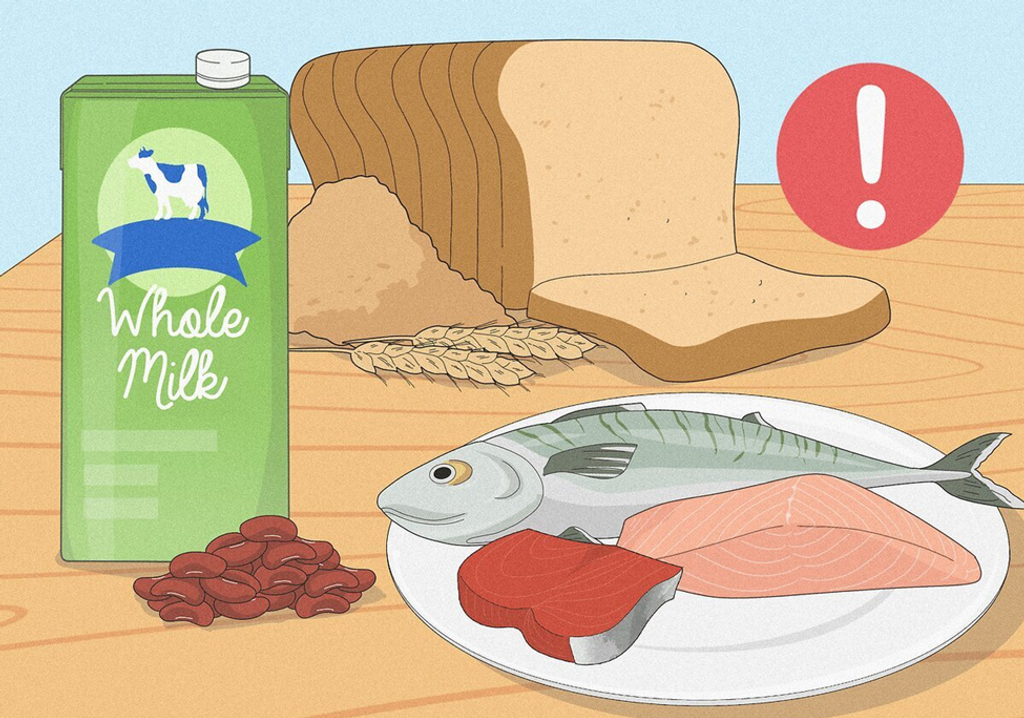
- Primary Trimethylaminuria (fish odor syndrome) is a metabolic disorder triggered by menstruation, specific medications, or choline-rich foods.
- More common causes of a fishy odor encompass inadequate hygiene, gingivitis, vaginosis, urinary tract infections, and advanced liver or kidney disease.
- The management of Trimethylaminuria involves dietary adjustments, using of mildly acidic soaps, avoiding certain medications, and potentially a brief regimen of neomycin or metronidazole.
Introduction on Fish Odor Syndrome
In 1970, Humbert and his team brought to the medical community’s attention a unique instance involving a 6-year-old girl who displayed clinical characteristics resembling those of Noonan’s syndrome, coupled with an unusual symptom: intermittent body odor resembling that of rotting fish [1]. This combination of symptoms marked the emergence of what would later become known as Trimethylaminuria, commonly called Fish odor syndrome.
It is a metabolic disorder characterized by abnormal excretion of trimethylamine in bodily fluids such as breath, urine, sweat, saliva, and vaginal secretions [2]. Trimethylamine is produced by intestinal bacteria from the breakdown of foods rich in choline and carnitine. Normally, the liver oxidizes trimethylamine into odorless trimethylamine N-oxide, which is excreted in urine [3]. However, impaired oxidation of trimethylamine leads to the characteristic smell of rotting fish associated with this syndrome. Certain choline-rich foods can exacerbate the condition, and affected individuals may experience various psychological issues [2,3]. Early recognition of the syndrome is crucial, as dietary modifications can reduce trimethylamine excretion and alleviate odor. In some cases, a brief regimen of metronidazole, neomycin, or lactulose may be prescribed to suppress trimethylamine production by decreasing the activity of gut microflora [4].
Prevalence and Etiology
Initially categorized as a rare condition, recent evidence challenges this perception, suggesting a higher prevalence than previously believed. Studies conducted across diverse populations, including those in Jordan, Ecuador, and Britain, have uncovered varying rates of compromised trimethylamine oxidation, indicating a wider range of affected individuals than previously recognized [2,9]. Trimethylamine, the unpleasant odor-causing agent in this syndrome, originates from the breakdown of foods rich in choline and carnitine, with fish being a significant source [4]. In individuals with Trimethylaminuria, deficient trimethylamine oxidase activity in the liver hinders the oxidation of trimethylamine, leading to its buildup and subsequent release in bodily fluids [10].
Understanding the Physiology
Trimethylaminuria arises due to mutations in the FMO3 gene, which encodes for the enzyme flavin-containing monooxygenase 3 (FMO3) [5,7]. This enzyme oxidizes TMA into its non-odorous form, trimethylamine-N-oxide (TMAO). When FMO3 is deficient or dysfunctional, TMA accumulates in the body, producing a characteristic fishy odor [9].
Clinical Manifestations
Trimethylaminuria is inherited in an autosomal recessive manner, with carriers estimated to comprise approximately 1% of the population [11]. Typically, affected individuals exhibit intermittent symptoms exacerbated by factors such as puberty, sweating, emotional stress, and dietary intake rich in choline. While clinical presentation commonly occurs in childhood, onset may vary, with some cases manifesting in infancy or adulthood [2,12]. The distinctive odor, akin to rotting fish, emanates from bodily fluids, including sweat, urine, saliva, and vaginal secretions. Notably, the condition can be exacerbated by certain medications, hormonal changes, and dietary factors [13].
Treatment Approaches
While there is currently no exact cure for Trimethylaminuria, ongoing research is exploring potential therapeutic strategies to enhance FMO3 activity or reduce TMA production [17,21]:
- Pharmacological Interventions: Investigational drugs targeting FMO3 expression or activity are being explored as potential treatment options. These include chaperone molecules that stabilize mutant FMO3 enzymes or modulators that enhance enzyme activity [17].
- Gene Therapy: Emerging gene-editing technologies such as CRISPR-Cas9 hold promise for correcting FMO3 gene mutations, offering a potentially curative approach for TMAU in the future [18].
- Microbiome Modulation: Manipulating the gut microbiota through probiotics or dietary interventions may influence TMA production and metabolism, offering a novel therapeutic avenue for managing Fish Odor Syndrome [19].
Management and Future Directions

Effective management of Trimethylaminuria necessitates a multidisciplinary approach, encompassing dietary modifications, personal hygiene practices, and psychological support [21]. Dietary restrictions targeting choline and carnitine-rich foods and supplementing choline-binding agents may attenuate trimethylamine production. Topical solutions containing activated charcoal or zinc can help mitigate odor, while psychological interventions, including counseling and support groups, are instrumental in addressing the psychosocial sequelae [15,16].
Conclusion
Trimethylaminuria goes beyond its simplified label of Fish Odor Syndrome, representing a multifaceted interaction of genetic predisposition, metabolic irregularities, and psychosocial implications. By clarifying its prevalence, causes, and clinical presentations, healthcare providers can embrace a more comprehensive approach to diagnosis, treatment, and patient support, enabling affected individuals to better cope with the challenges associated with this often-underestimated condition. As research efforts persist in uncovering the complexities of Trimethylaminuria, promoting increased awareness and comprehension is essential for cultivating a compassionate and inclusive healthcare environment for individuals impacted by this rare yet significant disorder.
References
- Humbert JR, Hammond KB, Hathaway WE, Marcoux JG, O’Brien D (1970). Trimethylaminuria: the fish-odor syndrome. Lancet ii: 770–771.
- Ayesh R, Mitchell SC, Zhang AQ, Smith RL (1993). The fish odor syndrome: biochemical, familial, and clinical aspects. BMJ 307: 655–657.
- Willey GR (1985) Trimethylaminea pungent experience. Educat Chem 22:178–181.
- Hadidi HF, Cholerton S, Atkinson S, Irshaid YM, Rawashdeh NM, Idle JR (1995) The N-oxidation of trimethylamine in a Jordanian population. Br J Clin Pharmacol 39(2):179–181.
- Mitchell SC, Zhang AQ, Barrett T, Ayesh R, Smith RL (1997) Studies on the discontinuous N-oxidation of trimethylamine among Jordanian, Ecuadorian, and New Guinean populations. Pharmacogenetics 7(1):45–50.
- Zhang AQ, Mitchell SC, Smith RL (1996) Discontinuous distribution of N-oxidation of dietary-derived trimethylamine in a British population. Xenobiotica 26(9):957–961.
- De La Huerga J, Popper H (1951) Urinary excretion of choline metabolism following administration in normal and patients with hepatobiliary disease. J Clin Invest 30:463–470.
- Higgins T, Chaykin S, Hammond KB, et al. (1972) Trimethylamine N-oxide synthesis: a human variant. Biochem Med 6:392–396.
- Al-Waiz M, Ayesh R, Mitchell SC, Idle JR, Smith RL (1987) A genetic polymorphism of the N-oxidation of trimethylamine in humans. Clin Pharmacol Ther 42:588–594.
- Growdon JH, Cohen EL, Wurtman RJ (1977) Huntington’s disease: clinical and chemical effects of choline administration. Ann Neurol 1:418–422.
- Marks R, Dudley F, Wan A (1978) Trimethylamine metabolism in liver disease. Lancet i:1106–1107.
- Fernandez MS, Gutierrez C, Vila JJ, et al. (1997) Congenital intrahepatic portocaval shunt associated with Trimethylaminuria. Pediat Surg Inter 12:196–197.
- Simenhoff ML, Ginn HE, Teschan PE (1977). The Toxicity of aliphatic amines in uremia. Trans Am Soc Artif Organs 23: 560–561.
- Wills MR, Savory J (1981). The Biochemistry of renal failure. Ann Clin Lab Sci 11: 292–299.
- McConnell HW, Mitchell SC, Smith RL, Brewster M (1997). Trimethylaminuria associated with seizures and behavioral disturbance: a case report. Seizure 6: 317–321.
- Brand JM, Galask RP (1986). Trimethylamine: the substance mainly responsible for the fishy odor often associated with bacterial vaginosis. Obstet Gynecol 68: 682–685.
- Pearson AW, Butler EJ, Curtis RF, et al. (1979) Effects of rapeseed meal on trimethylamine metabolism in domestic fowl in relation to egg taint. J Sci Food Agr 30: 799–804.
- Fenwick GR, Butler EJ, Brewster MA (1983) Are brassica vegetables aggravating factors in Trimethylaminuria (fish odor syndrome)? Lancet 2:916.
- Shelley ED, Shelley WB (1984) The fish odor syndrome. JAMA 251:253–255.
- Al-Waiz M, Ayesh R, Mitchell SC, Idle JR, Smith RL (1989) Trimethylaminuria: the detection of carriers using a trimethylamine load test. J Inher Metab Dis 12(1):80–85.
- Zhang AQ, Mitchell S, Smith R (1995) Fish odor syndrome: verification of carrier detection test. J Inher Metab Dis 18(6):669–674.
- Rithschild JG, Hansen RC (1985) Fish odor syndrome: Trimethylaminuria with milk as a chief dietary factor. Pediatr Dermatol 3:38–39.
- Pike MG, King GS, Pettit BR, Leonard JV, Atherton DJ (1988) Lactulose in Trimethylaminuria, the fish-odor syndrome. Helv Paediatr Acta 43:345–348.
- Wilcken B (1993) Acid soaps in the fish odor syndrome. BMJ 307:1497.
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!







