Lymphedema affecting the external genitalia is a rare condition characterized by swelling in the scrotal skin and underlying tissue due to impaired lymphatic drainage. Persistent cases can lead to fibrosis, significantly impacting the patient’s quality of life. While conservative methods are typically the initial approach, severe instances may require surgical intervention for lasting improvements.
We present the case of a 43-year-old overweight male who sought medical attention for ongoing bilateral scrotal swelling over three months. Clinical examination revealed a sizable, pressure-tolerant, soft scrotum enlargement on both sides. Ultrasound confirmed widespread thickening of the edematous scrotal wall. Despite recommendations for physiotherapy and conservative management, the patient opted for surgical excision of the scrotal swelling followed by scrotoplasty due to its debilitating size.
This case report delves into the presentation, symptoms, impact on patients’ lives, and diverse management options for scrotal lymphedema. It highlights the complexities in diagnosis and treatment decisions, emphasizing the necessity of a personalized and multidisciplinary approach.
Initial exclusion of life-threatening causes is crucial in ensuring optimal care for scrotal lymphedema. The incorporation of surgical interventions should be thoughtfully considered for a comprehensive management strategy, as scrotoplasty in the context of scrotal lymphedema not only enhances quality of life but also positively influences sexual function.
Navigating Isolated Scrotal Lymphedema: Introduction
Lymphedema, marked by an abnormal accumulation of lymphatic fluid, is characterized by persistent swelling in one or multiple areas, often accompanied by potential tissue alterations. The swelling can manifest in either proximal regions or distal extremities, presenting symptoms such as heaviness, pain, skin discoloration, restricted range of motion, and difficulty in ambulation [1,2]. Scrotal lymphedema, a rare condition, leads to swelling of the scrotal skin and subcutaneous tissue due to issues with lymphatic vessels, such as dysplasia or obstruction. Over time, fibrosis develops, negatively impacting the patient’s Quality of Life (QOL) [2,3]. The primary approach to managing this condition involves conservative methods, with physiotherapy particularly beneficial in the early and milder stages, ultimately enhancing QOL. Complex Decongestive Therapy (CDT), encompassing Manual Lymph Drainage (MLD), skin care management, therapeutic exercises, compression garments, bandaging treatment, and, crucially, self-education, is a key component of conservative therapy [4]. In cases where conservative management proves ineffective, surgical intervention may be considered. Timely diagnosis is imperative for proactive lymphedema management, effectively preventing and reducing the risk of recurrence [5]. This case report addresses idiopathic scrotal lymphedema, adhering to the SCARE Criteria [6].
Case Report
- Patient Profile:
- Age: 43
- Obesity Classification: BMI of 44.75 kg/m2
- Chief Complaint:
- Bilateral scrotal swelling.
- Onset: Three months ago.
- Extent: Enlarged to knees, causing walking difficulties.
- No associated scrotal trauma, urination issues, recent weight changes, or travel history.
- Medical History:
- No previous radiation exposure.
- Unremarkable past medical, family, and social history.
- Prior inguinal hernia repair with an unknown date.
- No history of lower urinary tract infections was reported.
- Medical Timeline:
- October 2022: Sought medical attention in Europe.
- Procedures: Methylene blue stain and scar release surgery.
- Outcome: Unsuccessful, persistent swelling.
- Within one year: Returned to Dubai outpatient clinic with recurrent swelling.
- Physical Examination:
- Swellings Characteristics: Pressure-indolent, soft, massively enlarged on both sides.
- Texture: Non-tender, non-pitting, non-reducible, fibrotic, and indurated scrotal tissue.
- Scars: Non-irritant thickened scars bilaterally in the groin.
- Penis: Retracted (Fig. 1, Fig. 2).

Fig. 1. Clinical scrotal appearance (standing view).
Fig. 2. Clinical scrotal appearance (supine view).
- Testicular Evaluation:
- Difficulty due to massive swelling.
- Normal external genitalia development.
- Transillumination tests: Negative for testicular swelling or hydrocele on both sides.
- Ultrasound (US) Findings: Significant diffuse edema in the entire scrotum. The left testicle was relatively small and hypoechoic, with a diffusely thickened edematous scrotal wall (Fig. 3).
- Doppler US: Good vascularity to both testes.
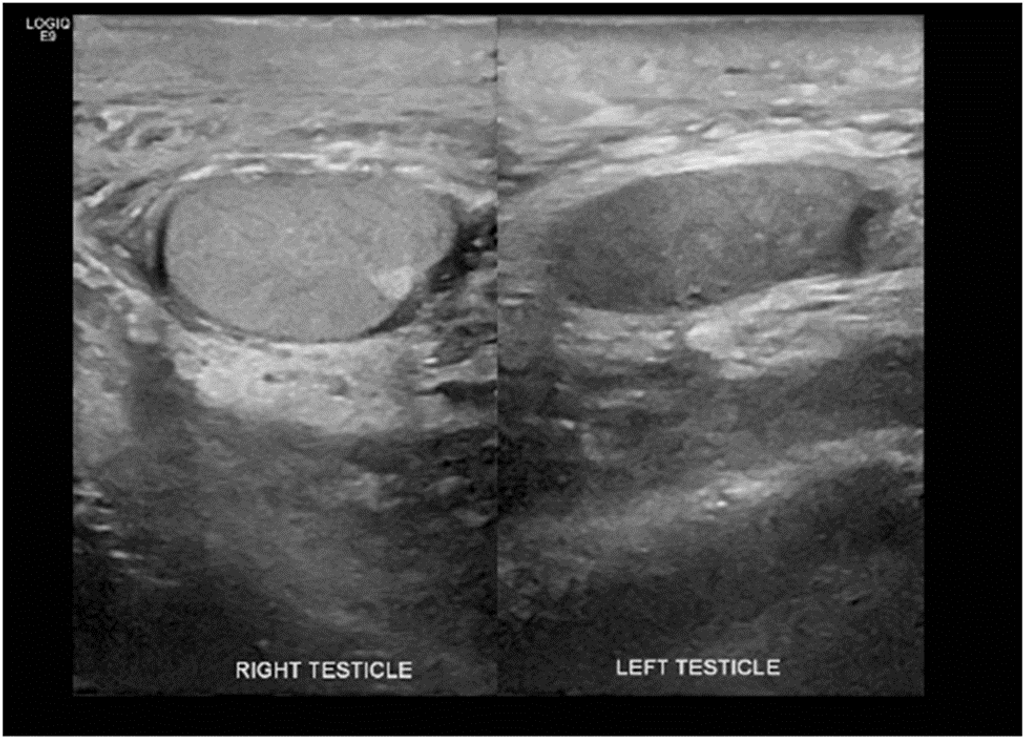
Fig. 3. Ultrasound of the testes.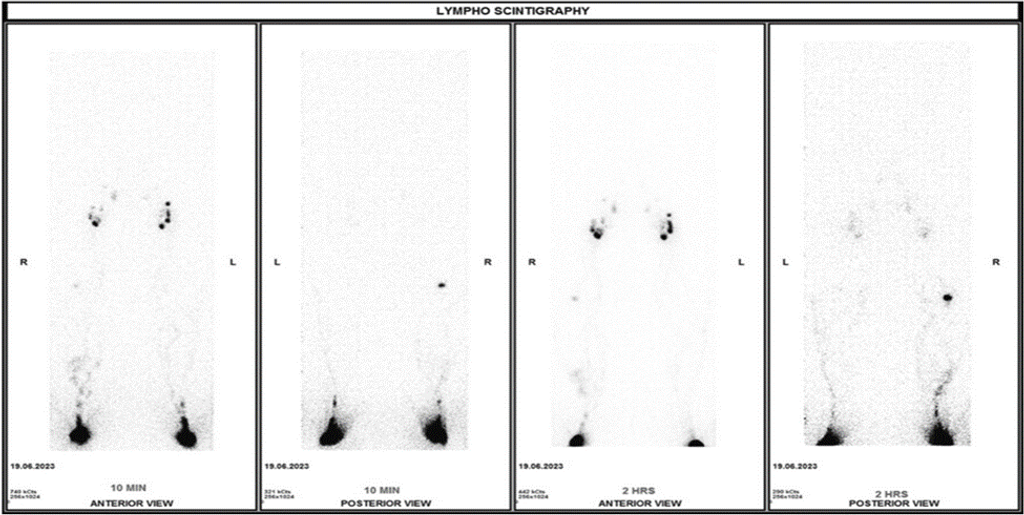
Fig. 4. Lymphoscintigraphy-T99m-NNC.
- Lymphatic Assessment:
- Lymphoscintigraphy-Tc99m-NNC scan.
- Findings: Persistent visualization of right popliteal lymph node, formation of collaterals (Fig. 4, Fig. 5).
- Interpretation: Suggestive lymph rerouting through the system, potentially leading to future lymphatic obstruction.
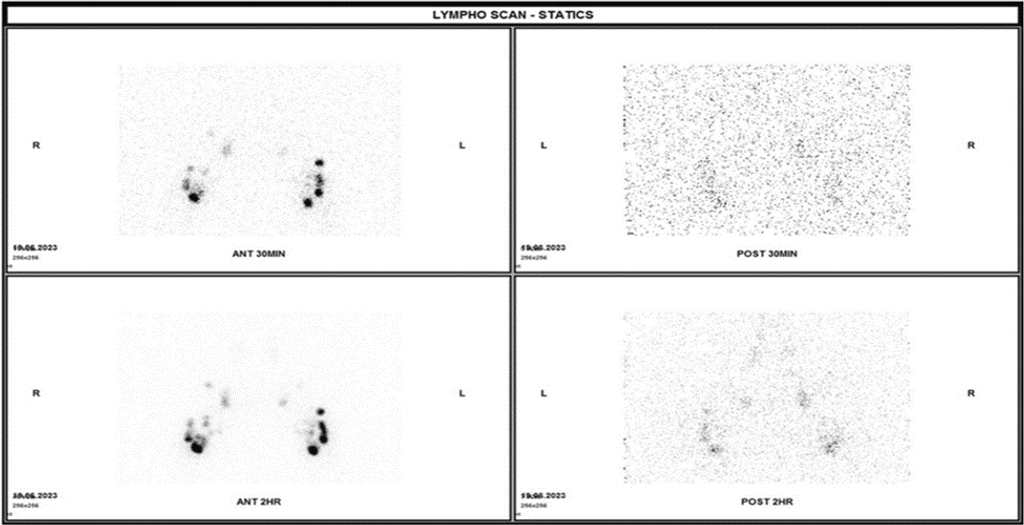
Fig. 5. Lymphoscintigraphy-T99m-NNC.
- Differential Diagnosis:
- Bilateral idiopathic scrotal lymphedema.
- Massive localized lymphedema was secondary to morbid obesity.
- Lymphatic filariasis.
- Lymphedema secondary to hernia repair surgery.
- Adult-acquired buried penis.
- Diagnostic Tests:
- Polymerase chain reaction tests (Negative for Treponema pallidum, Chlamydia trachomatis, and filarial antibodies).
- Tumor markers (Negative for total beta-human chorionic gonadotropin and alpha-fetoprotein).
- Preliminary Diagnosis:
- Bilateral idiopathic scrotal lymphedema, established after excluding other causes.
- Treatment Approach:
- Initial Recommendations: Weight loss attempts and Complex Decongestive Therapy (CDT).
- Response: Some improvement, but challenges in weight loss and ongoing swelling persisted.
- Mutual Agreement: Surgical intervention considered.
- Surgical Procedure (July 2023):
- Scrotal Excision Surgery:
- Incision: Median raphe incision from penis base to perineum.
- Preservation: Underlying structures (urethra, testicles, inguinal cords).
- Tissue Excision: Two wedge-shaped parts weighing approximately 1.3 kg.
- The largest piece measured 11.5 cm × 13.0 cm × 9.0 cm, and the smallest piece measured 9.0 cm × 5.5 cm × 2.5 cm, displaying a pale brown cut surface.
- Histopathology: Displayed edematous stroma, hypertrophied muscle bundles, lobular. Perivascular lymphocytes, plasma cell infiltrate, evidence of hemorrhage, and vascular congestion.
- Malignancy and Granuloma: Ruled out.
- Scrotoplasty: Inverse T-incision and suturing redundant skin for acceptable scrotal contour (Fig.6).

Fig. 6. Post-operative appearance.
- Scrotal Excision Surgery:
- Post-operative Care:
- Continued CDT sessions for ongoing lymphatic fluid transport enhancement.
- Post-Surgery Lifestyle Guidance:
- Focus on lifestyle adjustments emphasized.
- Key emphasis areas:
- Good personal hygiene
- Regular exercise
- Healthy eating habits
- Follow-up Appointment Details:
- Initially recommended after three weeks.
- Actual return after six weeks due to personal reasons.
- Post-Surgery Evaluation:
- Wound assessment:
- Successful healing observed
- No signs of infection
- Absence of lower urinary tract symptoms.
- Wound assessment:
- Unresolved Issue:
- Persistent buried penis noted.
- Challenges in sexual life reported.
- Quality of Life (QOL) Concerns:
- Normal bladder habits maintained.
- The patient expresses dissatisfaction with QOL after the surgical procedure.
Discussion
Scrotal lymphedema occurs when there is an abnormal accumulation of lymphatic fluid in the scrotal tissue stemming from compromised drainage. The broader classification of lymphedema includes primary and secondary types [7]. Primary lymphedema, resulting from malformations in the lymphatic system, comprises three subtypes: Congenital Lymphedema, evident at birth; Lymphedema Praecox, appearing during adolescence; and Lymphedema Tarda, emerging after the age of 35 [8]. On the other hand, secondary lymphedema, more common and occurring at any age, develops due to damage to the lymphatic system. It is associated with various underlying medical conditions or procedures, such as cancer treatment, trauma, obesity, chronic venous insufficiency, and infections like lymphogranuloma venereum and filarial infestation with Wuchereria bancrofti, particularly prevalent in tropical countries [3,8].
The escalating prevalence of lymphedema is closely linked to the rising incidence of morbid obesity, as evidenced by two notable studies [9]. In a 2014 study by Mehrara BJ et al., the reciprocal relationship between obesity and secondary lymphedema was underscored. This study revealed that obesity hampers lymphatic transport capacity, accumulating adipose tissue [1]. Furthermore, a 2022 study by Sudduth CL et al. found that obesity-induced lymphedema is more likely to occur with a BMI exceeding 40, and the likelihood significantly increases when the BMI surpasses 60 [10]. Noteworthy risk factors also encompass congestive heart failure and diuretic use. Clinically, scrotal lymphedema manifests as a large, painless, slow-growing soft tissue mass, causing discomfort, difficulties in ambulation, and cosmetic concerns. Fibrosis may lead to genital malformations that impact daily activities [2,9].
The diagnosis primarily relies on clinical assessment, although including ultrasound scans and magnetic resonance imaging may be considered to eliminate other potential causes. Unattended scrotal lymphedema, owing to its chronic and gradual progression, has the potential to diminish the patient’s quality of life substantially. It is imperative to provide lifelong care and psychosocial support [11]. Effectively managing chronic scrotal lymphedema necessitates a comprehensive strategy that combines conservative and surgical methods. A precise and timely diagnosis is crucial for the proactive management of lymphedema, aiming to prevent complications and reduce the risk of recurrence.
Achieving optimal outcomes in managing scrotal lymphedema involves implementing a comprehensive strategy that integrates conservative and surgical interventions. Regardless of the chosen approach, meticulous self-hygiene is imperative to prevent potential complications such as infections. Patient education, coupled with daily exercises like walking and using stairs, plays a pivotal role in the success of the treatment. It is essential to underscore the importance of adhering to recommended practices and fostering a comprehensive understanding of the chosen management strategy for optimal outcomes [12].
The main strategy for addressing scrotal lymphedema commonly revolves around conservative approaches, particularly physiotherapy techniques in the early and milder stages [4]. Conservative therapy follows a comprehensive method referred to as Complex Decongestive Therapy (CDT), which comprises two stages. In the initial stage, the emphasis is on skin care, Manual Lymph Drainage (MLD), muscle-pumping exercises, and compression therapy to enhance lymphedema volume. The second stage is centered on optimizing the outcomes achieved in the first stage and preventing complications through the ongoing application of techniques from the initial stage [12].
When conservative management falls short, the consideration of surgical intervention arises [12]. Surgical management can be categorized into physiological or reductive methods. Physiological methods enhance lymphatic drainage and reduce swelling through reconstructive procedures like Vascularized Lymph Node Transfer (VLNT) and Lymphaticovenular Anastomosis (LVA). VLNT involves transplanting healthy lymph nodes and associated blood vessels to the affected area, while LVA connects lymphatic vessels to nearby venules. Reductive methods target complications of lymphedema, such as lipodystrophy and fibrosis. In such cases, edematous and fibrotic tissue is either directly excised, ablated, or subjected to liposuction; it’s important to note that this method doesn’t restore lymph flow. A combination of physiological and reductive procedures can be employed in advanced stages for a more comprehensive and effective approach [5].
Patients dealing with scrotal lymphedema are encouraged to seek psychosocial support, including psychotherapy or consultations with psychologists, to enhance their overall Quality of Life (QOL).
Conclusion
The rare scrotal lymphedema, whether originating from primary or secondary lymphedema, requires timely diagnosis and intervention given its significant impact on patients’ Quality of Life (QOL), limiting their range of motion.
References
- G.T. Saeed, D. Ahmad, M.N. Al Smady, et al., Isolated scrotal lymphedema in a 43-year-old male patient: A case report, International Journal of Surgery Case Reports (2023), https://doi.org/10.1016/j.ijscr.2024.109403.
- Dayan JH, Ly CL, Kataru RP, Mehrara BJ. Lymphedema: Pathogenesis and Novel Therapies. Annu Rev Med. 2018 Jan 29; 69:263-276. doi: 10.1146/annurev-med-060116-022900. Epub 2017 Sep 6. PMID: 28877002.
- Akan S, Urkmez B, Artuk I, Urkmez A. Scrotal Lymphedema and its Conservative Treatment: A Rare Complication of Circumcision. J Coll Physicians Surg Pak. 2020 Jan;30(1):94 -95. doi: 10.29271/jcpsp.2020.01.94. PMID: 31931942.
- Pastor C, Granick MS. Scrotal lymphedema. Eplasty. 2011;11: ic15. Epub 2011 Nov 4. PMID: 22184510; PMCID: PMC3236059
- Istranov AL, Makarov IG, Makarova NV, Tulina I, Ulasov IV, Isakova YI. Combination of conservative and surgical methods in the treatment of giant lymphedema of the scrotum: A case report. Front Surg. 2023 Apr 12; 10:1048159. doi: 10.3389/fsurg.2023.1048159. PMID: 37123541; PMCID: PMC10130451.
- Sohrabi C, Mathew G, Maria N, Kerwan A, Franchi T, Agha RA. The SCARE 2023 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136.
- Sohrabi C, Mathew G, Maria N, Kerwan A, Franchi T, Agha RA. The SCARE 2023 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136.
- Vives F, García-Perdomo HA, Ocampo-Flórez GM. Giant lymphedema of the penis and scrotum: a case report. Autops Case Rep. 2016 Mar 30;6(1):57-61. Doi: 10.4322/acr.2016.026. PMID: 27284543; PMCID: PMC4880436.
- Grada AA, Phillips TJ. Lymphedema: Pathophysiology and clinical manifestations. J Am Acad Dermatol. 2017 Dec;77(6):1009-1020. doi: 10.1016/j.jaad.2017.03.022. PMID: 29132848.
- Bogusz AM, Hussey SM, Kapur P, Peng Y, Gokaslan ST. Massive localized lymphedema with unusual presentations: report of 2 cases and review of the literature. Int J Surg Pathol. 2011 Apr;19(2):212-6. doi: 10.1177/1066896908320833. Epub 2008 Jul 8. PMID: 18611926.
- Sudduth CL, Greene AK. Lymphedema and Obesity. Cold Spring Harb Perspect Med. 2022 May 27;12(5): a041176. doi: 10.1101/cshperspect. a041176. PMID: 35074795; PMCID: PMC9159261.
- 11. Casley-Smith JR. Alterations of untreated lymphedema and it’s grades over time. Lymphology. 1995 Dec;28(4):174-85. PMID: 8771010.
- Executive Committee of the International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2020 Consensus Document of the International Society of Lymphology. Lymphology. 2020;53(1):3-19. PMID: 32521126.
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!






