Non-Hodgkin’s Lymphoma (NHL) or Gastric Burkitt Lymphoma in individuals living with Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome (HIV/AIDS) remains a significant source of morbidity and mortality, displaying a propensity to manifest irrespective of the level of immunosuppression. Gastric Burkitt’s lymphoma emerges as a prominent subtype within this demographic.
This case report details the diagnosis of metastatic gastric Burkitt’s lymphoma in a 32-year-old man, discovered a month after his admission to a tertiary hospital for neurological symptoms. The primary objective of this study is to emphasize the importance of considering Burkitt’s lymphoma even in patients with robust immunity, thorough medical history, and comprehensive physical examinations, which constitute pivotal elements in achieving an accurate diagnosis.
Introduction: Gastric Burkitt Lymphoma in HIV/AIDS
Non-Hodgkin’s Lymphoma (NHL) in individuals living with Human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) (PLWHA) is a leading cause of elevated prevalence, morbidity and mortality, constituting 10% of cancers affecting PLWHA [1]. The systemic subtype associated with primary lymphoma of the central nervous system is a defining characteristic of AIDS, reflecting advanced immunosuppression [2]. Despite the heightened risk for those with a low CD4+ lymphocyte count and high viral load, the introduction of antiretroviral therapy (ART) has led to a gradual decline in the incidence of NHL in PLWHA [3,4]. However, Burkitt’s lymphoma may still affect up to 25% of patients with a CD4+ lymphocyte count exceeding 500 cells/microliter.
This study focuses on reporting cases of individuals with counts greater than 200 cells/microliter, particularly young individuals, highlighting the importance of clinical suspicion in the presence of symptoms indicative of the disease [4].
Case Presentation of Gastric Burkitt Lymphoma in HIV/AIDS [1]

Figure 1: Neuroaxis MRI Images
On neuroaxis MRI, multiple areas of osteolysis are evident in the bone marrow of the T11 vertebral body (A and C: indicated by yellow arrows, B: marked with red arrows). Additionally, osteolysis is observed in the sacral parts and iliac bones (B and C: denoted by red arrowheads). Accompanying this is a significant reduction in the height of the anterior aspect of the T11 vertebral body, exceeding 90%, and the presence of a collection with peripheral contrast enhancement extending into the pre- and paravertebral soft tissues at the T11 level (B and C: highlighted by red and yellow arrowheads). While the imaging pattern lacks specificity, it raises consideration for an association with the clinical suspicion of inflammatory/infectious involvement. The likelihood of a neoplastic nature is deemed less, though not entirely dismissible.
1. Patient Information: Age: 32-year-old man
- Symptoms:
- Unquantified weight loss
- Generalized lymph node enlargement
- Hypoesthesia
- Lower limb paresis
- Painless nodulation (4×3 cm) attached to the root of the left thigh.
2. HIV Diagnosis
- HIV diagnosed upon admission
- CD4 lymphocyte count: 99
- HIV viral load: 65
- Antiretroviral therapy (ART) started with a dolutegravir/lamivudine/tenofovir (TDF/3TC+DTG) combination.
3. Neuroaxis MRI Findings
- Sacral and iliac bone osteolysis
- Pathological fracture and T11 wedging
- Paravertebral collection with peripheral contrast enhancement
- Suggestive of infectious involvement
- The hypothesis of bone tuberculosis is considered (Figure 1).
4. Diagnostic Challenges: Sputum Investigation
- Negative results for real-time PCR-based rapid molecular assay and bacilloscopic
- The empirical treatment chosen for disseminated tuberculosis due to:
- Bone involvement
- Generalized lymph node enlargement
5. Reasons for Tuberculosis Diagnosis Pursuit
- Possibility of false negative test results in a highly prevalent country (Brazil)
- CD4 count lower than 200 (compatible with extra-pulmonary forms)
- Clinical and radiological presentation as contributing factors
- A biopsy of the thigh mass was performed.
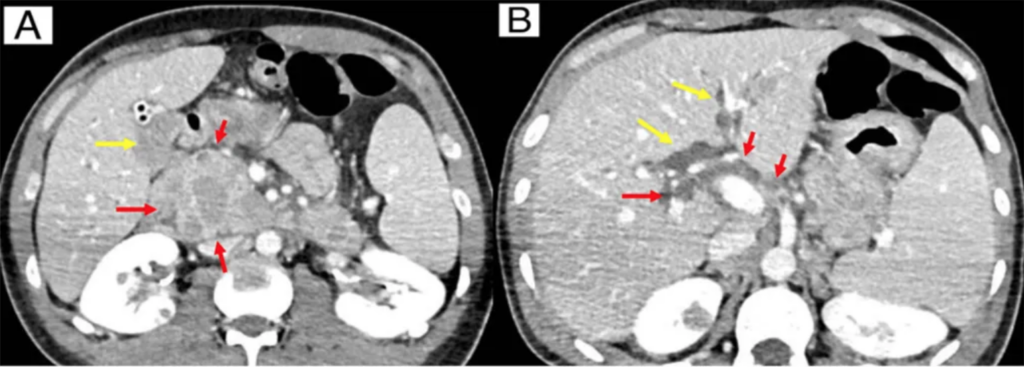
Figure 2: Abdominal CT scan images (axial view)
(A) The image shows dilation of the bile ducts (yellow arrows), probably due to compression, which may correspond to granulomatous diseases (red arrows), such as disseminated tuberculosis or neoplastic dissemination of Burkitt’s lymphoma. (B) The image shows multiple peripancreatic necrotic lymph node enlargements in the hepatic hilum (red arrows), exerting a compressive effect on the bile ducts.
6. Additional Complication
- Acute cholangitis developed 20 days after admission
- Abdominal CT revealed extrinsic compression of the bile duct from the Vater papilla (Figure 2).
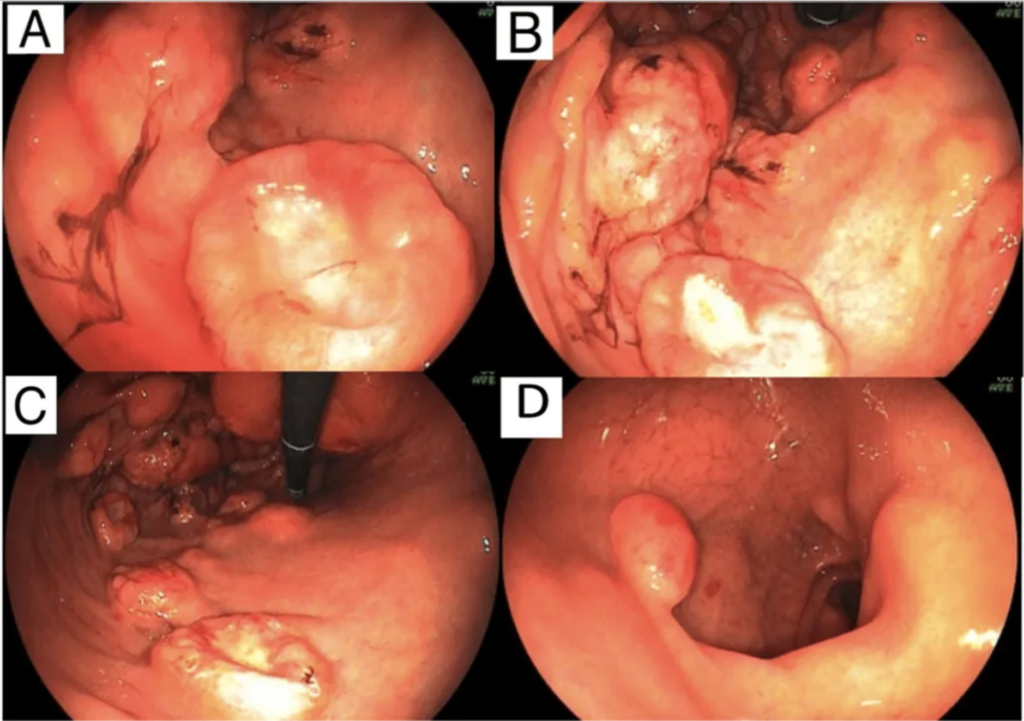
Figure 3: Upper Gastrointestinal Endoscopy Images
Upper GI shows, in the stomach, numerous elevated lesions, some with central ulceration, measuring between 10 and 25 mm, some of them friable, the largest located at the bottom, where there was still a bulge measuring around 3 cm (B and C). Such findings, on macroscopy, are compatible with extrinsic compression or submucosal involvement of findings compatible with lymphoproliferative or infectious diseases, such as lymphomas, Kaposi’s sarcoma or disseminated tuberculosis. Angular notch and antrum display flat-elevated lesions, reddish to burgundy, measuring between 6 and 10 mm (A). The duodenal bulb (D) shows two elevated lesions, measuring between 10 and 13 mm, with reddish surfaces located on the anterior and posterior walls
7. Upper Gastrointestinal Endoscopy (EGD) Findings
- Numerous elevated lesions in the stomach
- Some with central ulceration
- Others bulging in the fundus, body, and antrum region
- Two elevated reddish lesions in the duodenum
- Biopsies were performed on gastric ulcer and duodenal nodulation (Figure 3).
8. Subsequent Procedures
- Endoscopic ultrasound and endoscopic retrograde cholangiopancreatography
- Urgent drainage with the insertion of a plastic prosthesis in the bile duct
- Stable evolution post-procedure.
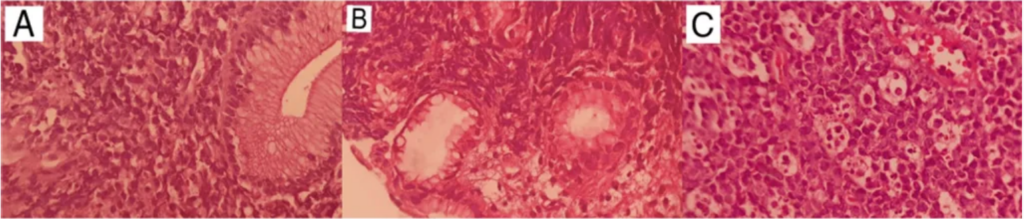
Figure 4: Histopathology Images
Magnification (H&E, 400X) shows atypical lymphoid cells surrounding and infiltrating duodenal (A) and gastric glands (B). Magnification shows sheets of monotonous intermediate-size cells with starry sky appearance in the inguinal lymph node (H&E, 400X) (C). Tingible body macrophages are phagocytic apoptotic debris.
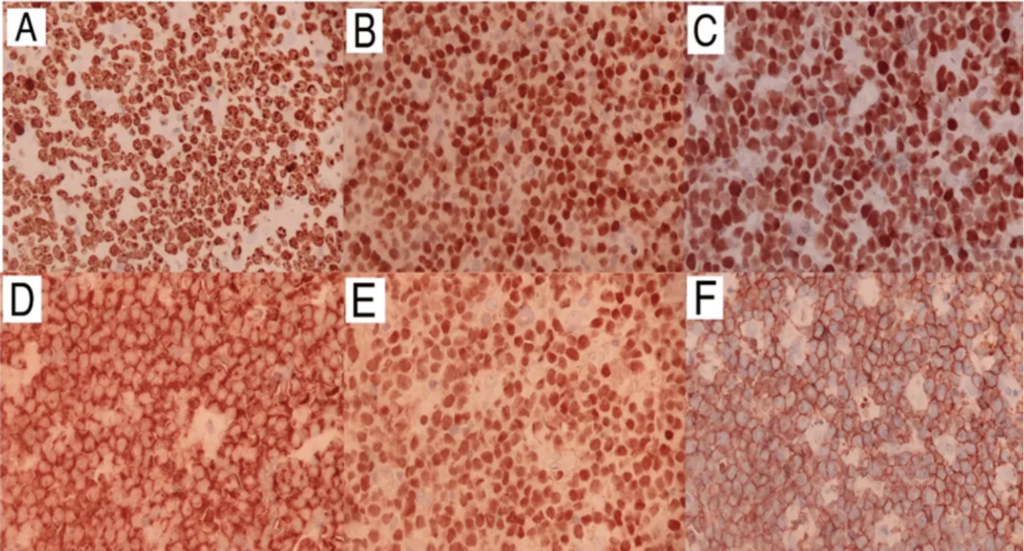
Figure 5: Immunohistochemistry Images
Immunohistochemistry images show tumor proliferation factor Ki67 approaching 100% (A), as well as positivity for markers cMYC (B), BCL6 (C), CD10 (D), PAX5 (E), and CD20 (F).
9. Gastrointestinal Biopsy Results
- High-grade non-Hodgkin lymphoma (NHL) detected during hospitalization
- The gastrointestinal tract and previously biopsied left lower limb mass showed the same pattern
- Positive immunohistochemistry for CD20, CD10, BCL6, CMYC, and PAX5
- Negative for BCL2, EBV, and TdT
- Ki67 of 100% (Figure 4 and Figure 5).
10. Burkitt’s Lymphoma Diagnosis
- Findings compatible with Burkitt’s lymphoma
- Initiation of chemotherapy with the cyclophosphamide, hydroxydaunorubicin, oncovin, and prednisone (CHOP) regimen
- Progressive clinical improvement.
11. Oncology Center Transfer
- The patient was transferred to an oncology center for specific treatment
- The decision to continue tuberculosis treatment until the investigation of previously described bone lesions concludes.
Discussion
In about 70% of patients, lymphomas in people living with HIV/AIDS (PLWHA) typically present with B-cell symptoms, such as fever, weight loss, night sweats, and lymphadenopathy. These manifestations can be easily confused with those seen in the general population. However, the distinction is made based on the frequency of extranodal involvement, particularly in areas like the gastrointestinal tract, liver, bone marrow, and central nervous system, which is more common in PLWHA [5-7]. The challenge lies in the nonspecific nature of these signs and symptoms, as they can be attributed to various comorbidities in immunosuppressed individuals. The specific case discussed here involves Burkitt’s lymphoma, an extranodal subtype of systemic non-Hodgkin lymphoma (NHL) categorized as aggressive. It holds the second-highest prevalence (25%) within the systemic NHL group [8].
The primary focus of the extranodal manifestation of non-Hodgkin lymphoma (NHL) is the involvement of the gastrointestinal tract. This characteristic highlights the inclusion of NHL in diagnostic considerations when faced with clinical syndromes resembling the presented case, given its aggressive nature and heightened risk of complications, particularly in people living with HIV/AIDS (PLWHA). Typically, the gastrointestinal tract is affected through secondary dissemination of lymphomas from a primary lymph node focus, with the stomach being the most commonly affected organ, followed by the duodenum and anal/perianal region, as observed in our patient. Primary presentation is uncommon, posing challenges in determining the primary site of disease involvement [9].
Gastric Burkitt’s lymphoma can imitate peptic ulcers, presenting with symptoms like dyspepsia and iron deficiency anemia, and may progress to pyloric obstruction [10]. Histologically, it exhibits monomorphic cells of medium size with a rounded nucleus, regular chromatin dispersion, and multiple small nucleoli. The presence of a “starry sky” pattern arises from the dispersion of macrophages containing phagocytosed material. The risk of obstruction, hemorrhage, and perforation increases when the intestine is affected.
Conclusion
In this case, report, while the initial focus was on neurological symptoms, it is crucial to note the presence of additional symptoms, such as lymph node enlargement and weight loss, aligning with the spectrum of complaints associated with lymphoproliferative neoplasms. The decision to conduct an upper gastrointestinal endoscopy in response to a clinical complication from the gastrointestinal (GI) system underscores the significance of considering this disease. Early suspicion is vital for prompt diagnosis, enabling the timely implementation of an appropriate therapeutic strategy.
References
- Razera R, Souza-Filho R, Patzina R, et al. (February 09, 2024) Lymph Node Penetration from Gastric Burkitt Lymphoma in a Patient Living With HIV/AIDS. Cureus 16(2): e53905. doi:10.7759/cureus.53905.
- Akanmu AS: AIDS-associated malignancies. Afr J Med Med Sci. 2006, 35 Suppl:57-70.
- Gérard L, Galicier L, Boulanger E, et al.: Improved survival in HIV-related Hodgkin’s lymphoma since the introduction of highly active antiretroviral therapy. AIDS. 2003, 17:81-7. 10.1097/00002030-200301030-00011.
- Burgi A, Brodine S, Wegner S, et al.: Incidence and risk factors for the occurrence of non-AIDS-defining cancers among human immunodeficiency virus-infected individuals. Cancer. 2005, 104:1505-11. 10.1002/cncr.21334.
- Yanik EL, Achenbach CJ, Gopal S, et al.: Changes in clinical context for Kaposi’s sarcoma and non-Hodgkin lymphoma among people with HIV infection in the United States. J Clin Oncol. 2016, 34:3276-83. 10.1200/JCO.2016.67.6999.
- Ferry JA: Burkitt’s lymphoma: clinicopathologic features and differential diagnosis. Oncologist. 2006, 11:375-83. 10.1634/theoncologist.11-4-375.
- Davi F, Delecluse HJ, Guiet P, et al.: Burkitt-like lymphomas in AIDS patients: characterization within a series of 103 human immunodeficiency virus-associated non-Hodgkin’s lymphomas. Burkitt’s Lymphoma Study Group. J Clin Oncol. 1998, 16:3788-95. 10.1200/JCO.1998.16.12.3788.
- Gabarre J, Raphael M, Lepage E, et al.: Human immunodeficiency virus-related lymphoma: relation between clinical features and histologic subtypes. Am J Med. 2001, 111:704-11. 10.1016/s0002-9343(01)01020-8.
- Loghavi S, Kanagal-Shamanna R, Khoury JD, Medeiros LJ, Naresh KN, Nejati R, Patnaik MM: Fifth edition of the World Health Classification of Tumors of the Hematopoietic and Lymphoid Tissue: myeloid neoplasms. Mod Pathol. 2023, 37:100397. 10.1016/j.modpat.2023.100397.
- Gormley RP, Madan R, Dulau AE, et al.: Germinal center and activated B-cell profiles separate Burkitt lymphoma and diffuse large B-cell lymphoma in AIDS and non-AIDS cases. Am J Clin Pathol. 2005, 124:790-8. 10.1309/7CEA-WV0D-NLLU-WQTF.
About Docquity
If you need more confidence and insights to boost careers in healthcare, expanding the network to other healthcare professionals to practice peer-to-peer learning might be the answer. One way to do it is by joining a social platform for healthcare professionals, such as Docquity.
Docquity is an AI-based state-of-the-art private & secure continual learning network of verified doctors, bringing you real-time knowledge from thousands of doctors worldwide. Today, Docquity has over 400,000 doctors spread across six countries in Asia. Meet experts and trusted peers across Asia where you can safely discuss clinical cases, get up-to-date insights from webinars and research journals, and earn CME/CPD credits through certified courses from Docquity Academy. All with the ease of a mobile app available on Android & iOS platforms!